While some of us may have a sweet tooth, the cells in our bodies definitely do not. Our cells naturally use a certain amount of glucose for fuel, but they’re not so keen on sweet-stuff overload. Consistently high levels of sugar in our bloodstreams make it tough for pancreatic cells to produce enough insulin. In response, the organ overcompensates by creating too much insulin and eventually becomes damaged (1). As blood sugar levels become consistently high, type-2 diabetes may develop.
There’s more bad news. Excess sugar in the bloodstream will injure other parts of the body, too. Its modified form becomes viscous and film-like, coating blood vessels and causing proteins to function poorly (1). For this reason, diabetics often experience other issues like kidney problems, vision loss, poor wound healing and nerve damage (i.e., neuropathy).
Given these issues—and the fact that 25+ million Americans have diabetes—it’s no wonder that the disease costs the country more than $116 billion annually in direct medical costs (1). Retailers should understand how to meet the needs of anyone concerned about healthy blood sugar levels, and be prepared to talk about how supplements and lifestyle choices play a role in glucose health.
If shoppers are looking for natural remedies for diabetes, let them know supplements can't be said to cure or prevent disease. Nonetheless, there are numerous natural ways to maintain healthy blood sugar levels.
Metabolic Syndrome Unraveled
 For some, learning of a blood sugar problem is followed by a landslide of diagnoses that no one wants to hear like high blood pressure, high cholesterol and too large a waistline. In short: metabolic syndrome, a predictor of serious problems like stroke and diabetes. The list of associated symptoms is growing, too. According to Michael T. Murray, N.D., director of product development for Natural Factors, Everett, WA, “The ‘controversy’ is whether other abnormalities such as chronic proinflammatory and prothrombotic states, non-alcoholic fatty liver disease and sleep apnea should be added to the syndrome, making its definition even more complex.”
For some, learning of a blood sugar problem is followed by a landslide of diagnoses that no one wants to hear like high blood pressure, high cholesterol and too large a waistline. In short: metabolic syndrome, a predictor of serious problems like stroke and diabetes. The list of associated symptoms is growing, too. According to Michael T. Murray, N.D., director of product development for Natural Factors, Everett, WA, “The ‘controversy’ is whether other abnormalities such as chronic proinflammatory and prothrombotic states, non-alcoholic fatty liver disease and sleep apnea should be added to the syndrome, making its definition even more complex.”
According to Matt Warnock, president of RidgeCrest Herbals, Salt Lake City, UT, “About 50% of heart disease patients have metabolic syndrome. The evidence on diabetes is even stronger: about 75% of diabetics have metabolic syndrome. Metabolic syndrome reflects a set of very real concerns that often accompany the Standard American Diet and deserves to be addressed.”
Not everyone is convinced, however, that this grouping of symptoms alone is an accurate predictor of future heart problems and diabetes. Mark J. Kaylor, vice president of education and research at Mushroom Wisdom, East Rutherford, NJ, says the framing of metabolic syndrome has been on shaky ground from the start. He states, “There were challenges to the validity of it being a central disease focus and compounding the question were several working definitions that were in use.”
Dallas Clouatre, Ph.D., research and development consultant to Jarrow Formulas, Los Angeles, CA, points out that a diagnosis of metabolic syndrome has gone beyond its original intention. Clouatre believes that the initial point was that a cluster of conditions were all derived from insulin resistance—a physiologic, not a disease, state. The commonality, he says, offers a “conceptual framework in which to place a substantial number of apparently unrelated biological events into a pathophysiological construct.”
But now, metabolic syndrome is a different animal. States Clouatre, “Clinicians for their reasons and pharmaceutical companies for their reasons turned this on its head such that the metabolic syndrome (a grouping of five or more criteria) became a clinical concept to be harnessed for the prediction of cardiovascular disease and a syndrome to be used as the basis of clinical intervention. A physiologic category was turned into a clinical category.”
 Also weighing in is Trisha Sugarek, B.S., M.S., director of research and development/national educator at Bluebonnet Nutrition Corporation, Sugar Land, TX. She says, “There is no question that these risk factors have a tendency to cluster, but what is controversial is that some studies/researchers report that the syndrome is imprecisely defined especially since the underlying pathophysiology of this ‘syndrome’ has remained unclear. Therefore, the assumption that metabolic syndrome is a useful marker for CVD and type -2 diabetes can and has been challenged.”
Also weighing in is Trisha Sugarek, B.S., M.S., director of research and development/national educator at Bluebonnet Nutrition Corporation, Sugar Land, TX. She says, “There is no question that these risk factors have a tendency to cluster, but what is controversial is that some studies/researchers report that the syndrome is imprecisely defined especially since the underlying pathophysiology of this ‘syndrome’ has remained unclear. Therefore, the assumption that metabolic syndrome is a useful marker for CVD and type -2 diabetes can and has been challenged.”
One problem with this is that some elements of metabolic syndrome, once fully developed, may not be rectified by only addressing insulin resistance. For instance, “once sustained hypertension develops, changes quite often take place directly in the endothelium and in kidney function that will continue the hypertension even if insulin levels are brought down,” says Clouatre.
Martie Whittekin, certified clinical nutritionist, nationally syndicated radio host and author of Natural Alternatives to Nexium, www.RadioMartie.com, adds another dimension: some aspects of metabolic syndrome are not 100% proven to be connected with heart attacks. Cholesterol is one factor. [This discussion will be flushed out completely in the WholeFoods Magazine Heart Health Editorial Series this coming June through October.] In addition, some feel the lab values used for blood tests—which lead to diagnoses—may be out of range. Again, not everyone agrees the parameters for cholesterol testing are appropriate.
Whittekin sums things up: “For several reasons, the effort to bundle various lab test readings into predictions may be an expensive moot point…Spending a lot of time and research dollars shuffling the labels strikes me as being a bit like rearranging the deck chairs on the Titanic. It just makes more sense to focus resources on helping people do a better job on the basics that are proven to improve health.”
To complicate matters, the medical community is diagnosing some individuals with prediabetes. This condition, which is distinct from metabolic syndrome, is used to classify those whose blood glucose levels are higher than normal, but not so high that they have type-2 diabetes.
Regardless of what it is called, says  Rhonda Witwer, senior business development manager of nutrition at National Starch Food Innovation, Bridgewater, NJ, “It is becoming more and more obvious that insulin resistance (loss of insulin sensitivity) is a crucial mechanism and improving it will be critical to improving numerous health conditions.”
Rhonda Witwer, senior business development manager of nutrition at National Starch Food Innovation, Bridgewater, NJ, “It is becoming more and more obvious that insulin resistance (loss of insulin sensitivity) is a crucial mechanism and improving it will be critical to improving numerous health conditions.”
Unfortunately, most physicians wait until blood sugar levels are abnormal before they look at insulin resistance. “By then, significant damage has already been done because the loss of blood sugar control (leading to the onset of type-2 diabetes) is the very last step in a long progression of increasing insulin resistance,” says Witwer.
No one will argue that any of the metabolic disease risk factors are problematic. But Kaylor adds that grouping these factors under the umbrella of metabolic syndrome may make some in the medical community put personalized care by the wayside. “For me,” he states, “whether or not they chose to put a label on it is pretty much irrelevant. Fundamentally, it is often the labeling of diseases that keeps people from being treated as unique biological beings.”
Here’s where a retailer can play an important role: making certain shoppers understand that a diagnosis of metabolic syndrome isn’t a one-way street to disease. Many, many important health and lifestyle choices can make the situation better. Says Steve Holtby, president and CEO, Soft Gel Technologies, Inc., Los Angeles, CA, “It is an opportunity for patients to intervene to delay the onset of diabetes, which will also lower the risk for other complications, such as coronary artery disease or stroke. There is considerable evidence suggesting that metabolic syndrome can be prevented with lifestyle changes—particularly losing weight, eating a healthy diet and getting regular exercise.”
In agreement is Craig Klein, MS, CNS, LN, national educator of Michael’s Naturopathic Programs, San Antonio, TX, who states, “Diagnosing metabolic syndrome may not be the most important issue. What may be more significant is becoming more aware of the factors that are used to diagnose it. By making positive, healthful changes in diet and lifestyle, improvements can be seen in these measurements. Everyone can become more proactively involved with his or her own healthcare.”
 Blood Sugar Support
Blood Sugar Support
Chances are you regularly field questions from shoppers looking for natural remedies for diabetes. While dietary supplements cannot treat diabetes or replace prescribed medication, some have much research backing for supporting blood sugar health. Clouatre provides a broad framework for how most work: increasing insulin output, improving insulin function and inhibit the digestion of carbohydrates and/or their uptake into the bloodstream.
Here are some standouts noted by those interviewed for this piece.
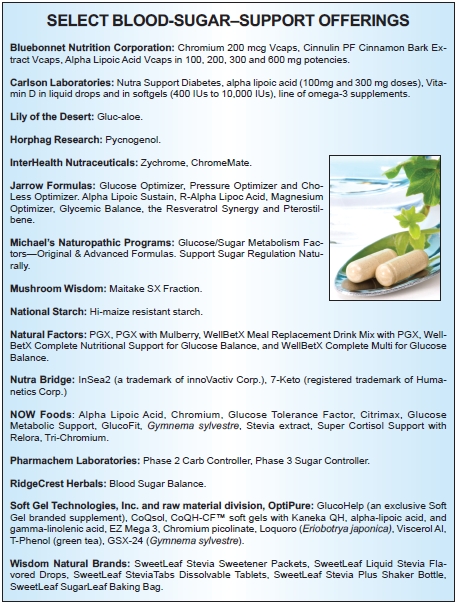
Cinnamon. A favorite among respondents was cinnamon, getting nods from many experts. Clouatre says cinnamon is an insulin sensitizer, and explains how it works: “Cinnamon may improve insulin resistance by preventing and reversing impairments in insulin signaling in skeletal muscle and by increasing the expression of peroxisome proliferator-activated receptors including PPAR-gamma in adipose tissue.” A 2011 study noted that this action is similar to how some diabetic drugs work (thiazolinediones). Fasting glucose levels are especially aided by cinnamon extract (2).
Sugarek also sheds some light on the use of cinnamon for blood sugar support: “Both test tube and animal studies have shown that compounds in cinnamon not only stimulate insulin receptors, but also inhibit an enzyme that inactivates them, thus significantly increasing cells’ ability to use glucose. Test tube, animal and human studies have all recently investigated cinnamon’s ability to improve insulin activity, and thus our cells’ ability to absorb and use glucose from the blood.”
Maitake. A specific fraction of the maitake mushroom (Maitake SX-Fraction) has been studied by Georgetown University and Shizuoka University. Researchers have found that this maitake component supports “healthy insulin function, glucose and lipid metabolism, blood sugar levels, cardiovascular function and body weight management,” according to Mushroom Wisdom, Inc.
Kaylor explains that the SX-Fraction benefits  healthy blood sugar in two ways: lowering both blood sugar and serum insulin. Research suggests that it may work by “improving cellular sensitivity to insulin, which can lessen the body’s demand for more insulin and help lower blood sugar levels,” according to Kaylor. This mechanism of action might be different from how other nutritional ingredients work. He states, “Many blood-sugar–lowering remedies work by stimulating insulin production, but for type-2 diabetics and metabolic syndrome sufferers, this may be problematic.”
healthy blood sugar in two ways: lowering both blood sugar and serum insulin. Research suggests that it may work by “improving cellular sensitivity to insulin, which can lessen the body’s demand for more insulin and help lower blood sugar levels,” according to Kaylor. This mechanism of action might be different from how other nutritional ingredients work. He states, “Many blood-sugar–lowering remedies work by stimulating insulin production, but for type-2 diabetics and metabolic syndrome sufferers, this may be problematic.”
Resistant starch. While some diabetics might be conditioned to avoid starch in any form, one branded starch may actually be beneficial. It’s true that the body breaks down many starches as sugar in the small intestine. But, resistant starches aren’t digested until they get to the large intestine, similar to a dietary fiber. There are two reasons why this is important in the context of blood sugar. Witwer explains that “(1) it reduces the glycemic response to foods, and (2) it helps to improve insulin sensitivity (i.e., reduces insulin resistance).”
Witwer speaks of her company’s branded resistant starch (Hi-maize), noting that more than 20 published human clinical trials connect it to a favorable glycemic and short-term insulin response. For instance, six show that Hi-maize resistant starch increased insulin sensitivity in adults. “These trials demonstrate that the consumption of modest levels of Hi-maize resistant starch can offer support in the pursuit of better glycemic health—both as a replacement for high-glycemic carbohydrates and as a standalone supplement to the diet. In particular, it can support healthy individuals and those at risk for prediabetes in maintaining healthy blood glucose levels and improve their overall glycemic health,” she explains.
A 2011 study of overweight men found a 50% increase in insulin sensitivity (3).
PGX. Many people concerned with stabilizing blood sugar also are looking for some sort of weight-management support. According to Murray, a dietary fiber matrix (PGX) has been linked to both.
 The matrix, he says, is a combination of natural soluble fibers (xantham gum, alginate and glucomannan) that make it “the most viscous and soluble fiber ever discovered.” The way it works is that PGX (taken as a supplement) forms a gel-like matrix in the body that expands and makes one feel full. It also slows digestion as well as the conversion of carbs into sugar. This means that glucose is released more gradually into the bloodstream. According to Murray, PGX “stabilizes blood sugar control in the overweight and obese”; “Reduces postprandial (after-meal) blood glucose levels when added to or taken with foods”; “Reduces the glycemic index of any food or beverage”; “Increases insulin sensitivity and decreases blood insulin”; “Improves diabetes control and dramatically reduces the need for medications or insulin in the diabetic”; and more.
The matrix, he says, is a combination of natural soluble fibers (xantham gum, alginate and glucomannan) that make it “the most viscous and soluble fiber ever discovered.” The way it works is that PGX (taken as a supplement) forms a gel-like matrix in the body that expands and makes one feel full. It also slows digestion as well as the conversion of carbs into sugar. This means that glucose is released more gradually into the bloodstream. According to Murray, PGX “stabilizes blood sugar control in the overweight and obese”; “Reduces postprandial (after-meal) blood glucose levels when added to or taken with foods”; “Reduces the glycemic index of any food or beverage”; “Increases insulin sensitivity and decreases blood insulin”; “Improves diabetes control and dramatically reduces the need for medications or insulin in the diabetic”; and more.
Murray notes that the supplement works best when used with a low-glycemic diet.
Chromium. Required for proper blood sugar management, “There is no underestimating the science behind chromium for blood sugar support,” says Paul Dijkstra, CEO of InterHealth Nutraceuticals, Benicia, CA. His firm surveyed 374 diabetes educators and more than 82% felt that chromium is necessary for insulin management.
According to Jolie Root, LPN, LNC, nutritionist and educator for Carlson Laboratories, Arlington Heights, IL, “Chromium enhances the action of insulin, likely by supporting the binding of insulin to insulin receptors.”
InterHealth has much clinical research indicating that its ChromeMate and Zychrome ingredients support blood sugar control, lipid modification and maintaining healthy body weight. For instance, studies say Zychrome improves insulin function and impacts insulin levels by 30% and was twice as effective as chromium picolinate.
Other chromium ingredients have research backing,  too. From Pharmachem Laboratories, Kearny, NJ, is Phase 3 Sugar Controller, which contains l-arabinose and a patented chromium. In a month-long clinical trial of 10 people, the ingredient showed a “statistically significant inhibitory effect on sucrose of 25%” (4).
too. From Pharmachem Laboratories, Kearny, NJ, is Phase 3 Sugar Controller, which contains l-arabinose and a patented chromium. In a month-long clinical trial of 10 people, the ingredient showed a “statistically significant inhibitory effect on sucrose of 25%” (4).
Aloe. Supplemental aloe is well recognized in the digestive care category, but it can also be helpful for those looking to support healthy blood sugar levels. One supplement (Gluc-aloe, from Lily of the Desert, Denton, TX) is made with a proprietary blend of polysaccharides from aloe vera. This formula has caught Whittekin’s eye. “A gold-standard, double-blind, placebo-controlled clinical trial showed that Gluc-aloe kept blood from sugar spiking after a meal,” she states. “Blood sugar measurements after meals improved a striking 72%...The cumulative effect of using a Gluc-aloe capsule before each meal for 90 days was that fasting blood sugars and the longer term measure of blood sugar stability, hemoglobin A(1c), returned to normal.”
Garlic. Often connected with heart health, garlic has been studied for benefits to diabetics. Root notes one study in which type-2 diabetics took garlic (or a placebo) along with a standard anti-diabetic drug (Metformin) (5). Those using the garlic supplement showed a “significant reduction in fasting blood sugar and a considerable decrease in mean total cholesterol, LDL cholesterol, triglycerides, while HDL cholesterol was significantly increased compared to Group 2. The combination of garlic with [diabetic drug] Metformin has shown to improve glycemic control in addition to antihyperlipidemic activity,” says Root.
 Gymnema sylvestre, banaba leaf, stevia, loquat. Another old standby comes from the herb department. Gymnema sylvestre is said to be one of the best-researched herbs for glucose support by increasing insulin release, which can benefit blood sugar regulation.
Gymnema sylvestre, banaba leaf, stevia, loquat. Another old standby comes from the herb department. Gymnema sylvestre is said to be one of the best-researched herbs for glucose support by increasing insulin release, which can benefit blood sugar regulation.
Neil E. Levin, CCN, DANLA, nutrition education manager for NOW Foods, Bloomingdale, IL, weighs in with info on this and other herbs: “For herbs, the best evidence is for them helping to maintain insulin sensitivity, control sweet cravings, and perhaps to support healthy pancreatic function: Gymnema sylvestre and Stevia rebaudiana (steviosides; not Reb A) appear to help us to manage healthy glucose metabolism, while Banaba leaf extract is a source of corosolic acid, which appears to aid in maintaining healthy insulin sensitivity.”
Holtby seconds the idea of banaba leaf (Lagerstroemia speciosa) for blood sugar support. The leaves contain corosolic acid and tannins, which are said to be beneficial to diabetics. Says Holtby, “A crossover five-month clinical trial involving type-2 diabetics demonstrated that GlucoFit (another extract from Lagerstroemia speciosa) significantly reduced blood glucose levels and supported small, but significant weight loss. GlucoFit also showed a ‘memory effect’ of blood glucose-lowering for a few days, even after the treatment was stopped.”
Also containing corosolic acid is loquat (Eriobotrya japonica), “a phytochemical known to activate facilitative blood glucose transporters,” says Holtby. “These carrier proteins help utilize glucose more efficiently without causing hypoglycemia.”
Alpha-lipoic acid. This antioxidant has a strong track record in diabetes use. Cells use alpha-lipoic acid to turn glucose into energy (6). “Supplementation with 600 mg daily has been shown to increase insulin sensitivity in patients diagnosed with type-2 diabetes (7),” says Root, adding, “It also has slowed the progression of diabetic nephropathy.”
Holtby adds that ALA may benefit diabetic neuropathy, “a painful condition that may be caused by elevated levels of free radicals which cause nerve and blood vessel damage.” In a review of 15 clinical trials (8), “The researchers concluded that three-week treatment using 600 mg per day of the ingredient reduced the chief symptoms of diabetic neuropathy.”
Sugarek adds some information on the R-lipoic acid form, which she says may help manage diabetic neuropathy: “free R-lipoic acid may enter nerve tissue and prevent glucose-related oxidative damage…R-lipoic acid oddly functions similarly to biotin; rotating one active site to another on a multi-subunit enzyme. In heavy metal intoxications, free lipoic acid and its metabolites are able to trap the metals in the circulation; thereby, preventing the damage caused by the metal and (sometimes) improving insulin’s secretion.”
White kidney bean extract. A natural extract of the white kidney bean (Phaseolus vulgaris) also has research backing for reducing carb and sugar digestion and uptake, says Clouatre. He says the ingredient is ”often suggested as a carb blocker to reduce blood glucose levels.”
One branded ingredient that falls under this umbrella is Phase 2 Carb Controller from Pharmachem Laboratories, which the company says is “clinically shown to reduce carb calories.” A research group lead by Jay Udani, M.D., gave the supplement (1,500 mg, 2,000 mg and 3,000 mg in powder and capsules) to subjects along with white bread. They found, “Reductions in the glycemic index of Wonder Brand white bread were seen at all dosages and formulations except the 1,500-mg capsule dose. These reductions reached statistical significance with 3,000 mg of Phase2 in powder form (-20.23 or  34.11%, p=0.0228) (9).”
34.11%, p=0.0228) (9).”
Brown seaweed extract. InSea2 (a trademark of innoVactiv Corp. and available from Nutra Bridge) was flagged by Clouatre for its ability to inhibit both starch and sucrose digestion. In a human clinical trial, subjects that took InSea2 (500 mg) a half-hour before eating white bread had a slower and more moderate change in blood glucose level than those taking a placebo.
Scott Steil, president of NutraBridge, Shoreview, MN, adds that InSea2 is the “only commercially available product that significantly blocks both alpha amylase and alpha-glucosidase enzymes (meaning that it blocks the breakdown of both starch and table sugar). As a result, it offers more complete control of blood sugar levels versus more traditional starch and carb blockers.” He believes supplementing with this ingredient will reduce quick spikes in blood glucose and insulin associated with consuming alpha amylase and alpha glucosidase enzymes.
Ginseng. Warnock supports the use of Traditional Chinese Medicine (TCM) for blood sugar support. TCM formulas contain interlocking herbs that work in conjunction with each other. In the glucose-support category, such formulas may contain ginseng. RidgeCrest Herbals use the Eleuthero root in its Blood Sugar Balance supplement, says Warnock, which “is an adaptogen that has been studied specifically for its effects in promoting healthy blood sugar regulation.”
Whittekin speaks of American ginseng, which has been known to create a 27% reduction in blood sugar spiking after meals. She adds, “While there are hints that American ginseng might help protect the beta cells of the pancreas, there is also some concern that it might increase oxidative stress in post-menopausal women (10).”
Pine bark extract. Research journals have featured a branded extract of the French maritime pine tree (Pycnogenol from Horphag Research) for its use in blood sugar care. In 2007, Diabetes Research and Clinical Practices published a study showing that the extract inhibited alpha-glucosidase, an enzyme that breaks down complex carbohydrates into glucose (11).
 Diabetes and Nutritional Deficiencies
Diabetes and Nutritional Deficiencies
While diabetics may focus on what they’ve eaten too much of (sugar, white carbs etc.), they should also consider what they may have consumed too little of.
For instance, researchers believe there is a strong relationship between low vitamin D levels and poor blood sugar regulation. Root of Carlson Labs notes “vitamin D plays a role in insulin secretion,” and points to a 2011 study in which low vitamin D levels was seen as a risk factor for developing type-2 diabetes (12).
The vitamin B complex also may be affected by blood sugar levels. Clouatre adds that deficiencies in biotin (B7) and vitamin B6 have been implicated in blood sugar issues. Another interesting point to consider comes from Holtby, who states that some oral medications often prescribed to diabetics may deplete folic acid and vitamin B12 levels. Customers taking these drugs (which include Glucophage, DiaBeta, Micronase and Glucotrol) may want to consider supplementing, with the permission of a physician, as well as taking a good multivitamin/mineral.
Indeed, mineral deficiencies may also be linked to blood sugar problems. According to Dijkstra, chromium is one to watch for. This trace element is needed for healthy protein, fat and carbohydrate metabolism, he says, adding that “it helps the body use insulin, which transfers blood sugar to the cells, where it is stored or burned as fuel.”
As we age, our chromium levels decline and our diets often lack chromium. Plus, certain groups of people (such as athletes, pregnant women and the elderly) are often prone to chromium deficiency. This is a problem, says Dijkstra, because the mineral is necessary for maintaining blood sugar control, heart health and a healthy weight, among other benefits.
Whittekin adds that other research (13) found “chromium deficiency in diabetics might be due to mineral losses from kidney damage but that chromium supplementation for those with insulin-resistance was likely protective.”
Another key mineral, according to Klein, is zinc because the pancreas needs it to make insulin. Insufficient zinc levels may cause insulin to drop too low. He adds, “It may become difficult to get glucose into the cells to be used as fuel. Inadequate consumption of chromium could have a negative impact on carbohydrate metabolism. This, again, could impact the amount of energy available to the cells.” Magnesium, too, is said to be important for blood sugar support.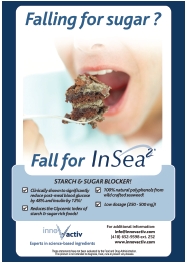
Despite the link between nutritional deficiencies and some nutrients, experts warn that one cannot overlook the fact that over-consumption is what caused some blood sugar problems to begin with.
Holtby says our habit of eating three large meals each day is also problematic because it can cause blood glucose levels to fluctuate too much. “This pattern of eating promotes chronic low blood sugar (hypoglycemia), which tricks the body’s biochemistry into thinking that it is in ‘starvation mode.’ The cells then become efficient at storing fat instead of burning fat.”
He notes that regular exercise paired with a high-fiber diet and a low-saturated and low-trans–fat diet can help. Also be sure to talk to clients about the fact that low-carb isn’t necessarily the way to go for everyone. Yes, eating too many white grains and sugary foods is going to lead to problems since they make glucose levels spike and crash quickly. But, a small amount of complex carbs release energy slowly and steadily.
Talking about Diabetes in Your Store
In May 2010, when the infamous Examples of Deceptive or Questionable Marketing Practices and Potentially Dangerous Advice report was made public by the U.S. Government Accountability Office (GAO), it became immediately clear that some supplement sellers were illegally telling shoppers that their products cured disease and medications weren’t needed. One disease caught in the crossfire was diabetes.
“Retailers must be very careful when talking with clients about diabetes or any disease. The U.S. Food and Drug Administration and the American Medical Association can construe giving advice as practicing medicine without a license,” says James May, founder and CEO of Wisdom Natural Brands, Gilbert, AZ. The topic of natural remedies for diabetes is tricky.
 So, what’s a retailer to do when a shopper asks for help with his/her diabetes?
So, what’s a retailer to do when a shopper asks for help with his/her diabetes?
What not to say. First and foremost, talking about supplements treating diabetes is never appropriate—no matter how enthusiastic you may be about an ingredient or finished product. This verbiage is illegal; supplements cannot claim to treat, prevent or mitigate any diseases. Adds Clouatre, “Although a product label may indicate ‘support for blood sugar already in the normal range,’ going beyond this level also is to make a disease claim.”
Steil offers another jumping off point: “Better to focus on products that help maintain healthy blood glucose and insulin levels.”
Witwer recommends being careful about using the glycemic index as a hard-and-fast benchmark for all diabetics. She notes, “Lowering the glycemic impact or response of foods does not correlate to reduced risk of diabetes.” For instance, replacing carbs with saturated fat for taste may lower its glycemic index or load, but it may not do much for one’s health. Rather, she says that replacements in recipes must be evaluated for appropriateness for blood sugar support on a case-by-case basis.
May seconds this practice, noting that shoppers should be trained to be careful label readers. For example, he says this is especially important because different products may use different “carriers” for stevia extract. “Because stevia extract is so intensely sweet, a carrier must be used and some manufacturers use another form of sugar as the carrier in their stevia sweetener,” May states. “If the customer asks about stevia, respond that it is your understanding that stevia does not increase blood sugar levels but advise them to read the label to understand what other ingredients or sweeteners may be in the product and always that the customer should discuss specific questions with his/her physician.”
Also not fit for discussion with customers is a comparison of supplements and medications. States Whittekin, “Never, ever, say that a supplement is better than so-and-so drug.” You don’t know a customer’s health history, even though you may have known the person for years; encouraging him or her to disobey a doctor’s orders could be dangerous.
Similarly, if a customer comes to you with symptoms or suspicions about an undiagnosed condition, stop them and tell them to see their healthcare provider. States Klein, “The clerk must avoid the temptation to diagnose the customer, telling him or her that he or she has a blood sugar problem. It is equally important not to state that any product will ‘fix the problem.’”
Levin wholeheartedly agrees on this front, noting, “Retailers have one thing that they can tell customers who have diabetes: that they should consult their physician before taking any supplements.”
What not to forget to say. Add to your “must say” list that shoppers should always follow the advice of a physician or a qualified health professional. This is very important because dietary changes—even moving to a whole food diet—“can be risky if a set dose of medicine is taken because less of the drug may then be needed, opening the door to a real risk of a drug overdose,” says Levin.
Clouatre says that “medications typically are designed to work within ranges of blood sugar excess and can readily cause low blood sugar if used outside the expected range.” So, if a supplement causes a person’s fasting blood sugar to drop, “the prescribed medication may now be too strong for the meals normally eaten.” In addition to letting a doctor know about new supplements, he suggests that blood sugar levels be monitored regularly and recorded. He adds, “A supplement that may make little difference at the end of the first week may make a lot of difference at the end of the first month.”
Witwer suggests making customers aware of the importance of understanding insulin resistance/insulin sensitivity. Murray calls insulin resistance the “greatest threat to the health of most Americans…Insulin resistance is the key underlying factor that leads to weight gain, the inability to lose weight, increased risk for heart disease, and the development of type-2 diabetes.” This biomarker, Witwer feels, is understood by public health authorities to affect prediabetes and type-2 diabetes. She says individuals have some level of insulin resistance if they can’t manage their blood sugar and weight by changing their carbohydrate intake. She adds, “Consumers should not wait for their blood sugar levels to rise before they start to manage their glycemic health. Instead, they should consider adding dietary ingredients that increase insulin sensitivity.”
But, shoppers aren’t as well-versed in its ins and outs, and may need more education about it. For starters, Murray reminds us that insulin resistance is tied to abdominal obesity. He states, “As fat cells in the abdomen grow in size or number, they secrete a number of biologic products (e.g., resistin) that dampen the effect of insulin, impair glucose utilization in skeletal muscle, and promote glucose (blood sugar) production by the liver. The net effect of all of these actions by fat cells in the overweight individual is that they severely stress blood sugar control mechanisms, as well as lead to the development of cardiovascular disease.”
 As for diet advice, May reminds that “a healthy diet and appropriate exercise are beneficial for everyone.” Escort customers to your appropriate supplements and foods section, suggesting that “sweeteners should only be used if they are low to zero calories,” he states.
As for diet advice, May reminds that “a healthy diet and appropriate exercise are beneficial for everyone.” Escort customers to your appropriate supplements and foods section, suggesting that “sweeteners should only be used if they are low to zero calories,” he states.
For supplements, Levin recommends sticking with “careful descriptions as to how certain products may support blood sugar already within the healthy range by the various mechanisms.”
Warnock adds that when talking about ways to “keep blood sugar levels within the normal range” and maintain “glucose health,” “store owners can certainly point out information that is readily available on the Internet and in many magazine articles,” he states.
Steil notes that this can be a big advantage for retailers, since he believes consumer awareness about nutraceutical options for blood sugar health is low. “To drive growth in the market segment,” he feels, “a strong educational push needs to happen...Also, retailers could dramatically expand the product offering in their store to help provide better solutions to those consumers who are battling metabolic syndrome. More ‘real estate’ for this category at the retail level will help drive consumer awareness.”
What to be sensitive about. Since type-2 diabetes is so commonly referred to as the result of poor diet and exercise habits, shoppers may be embarrassed, defensive or in denial about their condition. “Customers don’t want to be wrong, even if their choices have made them sick,” says Whittekin. Rather, she suggests displacing the blame a bit so they will be more open to hear about healthy lifestyle choices going forward. “It saves face a little bit for them to acknowledge that we’ve all been misled by ‘experts’ (e.g., food pyramid), mass market food manufacturers (e.g., selling us addictive junk food and making it sound healthful) and the media which can make lots of money selling advertising for sodas and drugs and none from farmers who grow organic broccoli.”
Warnock shares a similar opinion, noting that much of what’s on mainstream supermarket shelves has been created with dollars—not health—in mind. “Customers should know that over 100 years of food science has been developed specifically with the goal of increasing the sales of processed and branded foods. Creating healthy options has been a recent development,” he states. “Given that the playing field has been so heavily tilted for so long, customers should not blame themselves—we are all products of our economic culture to some extent. The important thing is to recognize the effect of these predispositions, and to work to offset and replace them with more healthy habits.”
Others feel that some tough love is in order, and prefer to speak about lifestyle changes openly.
You can also make the case that everyone—those diagnosed with diabetes or not—need to think about blood sugar health. Says Dijkstra, “One misconception among the general consumer population is that managing blood sugar is an isolated idea that only applies to people with diabetes. It is important to educate consumers so they recognize that even if they do not have any form of diabetes, it is critical to manage blood sugar levels to help interfere with metabolic pathways that may lead to excess body weight or cardiovascular issues.”
Be both optimistic and realistic. Even small lifestyle changes can positively affect blood sugar health, but Clouatre reminds us that some nutritional approaches take time—weeks or even months— before results are realized. Be sure to tell shoppers to be patient, and that believing natural remedies for diabetes exist to cure or preventative the disease is wrong.
Above all, says Klein, be empathetic, but don’t pry into areas where the shopper seems uncomfortable. He states, “Let the customer set the boundaries.” WF
References
1. WebMD, “How the Blood Sugar of Diabetes Affects the Body,” http://diabetes.webmd.com/how-sugar-affects-diabetes?page=2, accessed Dec. 28, 2011.
2. H. Rafehi, K. Ververis and T.C. Karagiannis, “Controversies Surrounding the Clinical Potential of Cinnamon for the Management of Diabetes,” Diabetes, Obesity and Metabolism, (2011) doi: 10.1111/j.1463-1326.2011.01538.x.
3. K.C. Maki, et al., “Effects of Type 2 Resistant Starch Consumption on Insulin Sensitivity in Men and Women,” #587.9 Poster presented at Experimental Biology, April 10, 2011.
4. G.R. Kaats, et al., “A Pilot Study of the Effects of L-A/Cr: A Novel Combination of L-Arabinose and a Patented Chromium Supplement on Serum Glucose Levels After Sucrose Challenges,” 2009.
5. R. Ashraf, R.A. Khan and I. Ashraf, “Garlic (Allium sativum) Supplementation with Standard Antidiabetic Agent Provides Better Diabetic Control in Type 2 Diabetes Patients,” Pak. J. Pharm. Sci. 24 (4), 565–570 (2011).
6. University of Maryland Medical Center, “Alpha Lipoic Acid,” www.umm.edu/altmed/articles/alpha-lipoic-000285.htm, accessed Dec. 29, 2011.
7. “Effects of Dietary Supplementation of Alpha-Lipoic Acid on Early Glomerular Injury in Diabetes Mellitus,” J. Am. Soc. Nephrol. 12 (1), 124–133 (2001).
8. D. Ziegler, et al., “Alpha-Lipoic Acid in the Treatment of Diabetic Polyneuropathy in Germany: Current Evidence from Clinical Trials,” Exp. Clin. Endocrinol. Diabetes. 107(7), 421–430 (1999).
9. J.K. Udani, M.L. Hardy and S. Shrestha, “A Novel Method of Lowering the Glycemic Index of White Bread Using a White Bean Extract,” (2007).
10. J.R. Dickman, “American Ginseng Supplementation Induces an Oxidative Stress in Postmenopausal Women,” J. Am. Coll. Nutr. 28 (2), 219–228 (2009).
11. A. Schäfer and P. Högger, “Oligomeric Procyanidins of French Maritime Pine Bark Extract (Pycnogenol) Effectively Inhibit alpha-Glucosidase,” Diabetes Res. Clin. Prac. 77 (1) 41–46 (2007).
12. B. Thorand, et al., “Effect of Serum 25-Hydroxyvitamin D on Risk for Type 2 Diabetes may be Partially Mediated by Subclinical Inflammation: Results from the MONICA/KORA Augsburg Study,” Diabetes Care 34 (10), 2320–2322 (2011).
13. S.M. Bahijri, E.M. Alissa, “Increased insulin resistance is associated with increased urinary excretion of chromium in non-diabetic, normotensive Saudi adults,” J Clin Biochem Nutr. 49(3), 164-8 (2011).
Published In WholeFoods Magazine, February 2012