Unfortunately, that’s very far from the whole story.
Pre-diabetes isn’t “just” pre-diabetes. It’s also pre-heart disease, pre-Alzheimer’s and pre- a whole lotta other chronic diseases. In fact, pre-diabetes—also known more accurately as insulin resistance syndrome—affects no less than 88% of Americans (1). And insulin resistance—which most people have never heard of and which most doctors are clueless about treating—underlies virtually every chronic disease we know of: diabetes, obviously, but also Alzheimer’s (which is now being referred to as Type lll Diabetes), heart disease, obesity, and lung, liver, and kidney disease (2,3).
Insulin resistance—not coincidentally, in my opinion—also underlies every single co-morbidity for COVID-19, excepting mental illness and socio-economic risk factors (4,5,6).
What’s more—as cardiologist Steven Sinatra and I argued in the revised edition of The Great Cholesterol Myth (7)—insulin resistance shows up years before your doctor tells you “Mrs. Jones, you have high blood sugar” or “Mr. Jones, you’ve got high cholesterol.” It’s one of the earliest identifiable risk factors for heart disease, and yet no one in conventional medicine is even talking about it.
And this is the kicker: Insulin resistance can be prevented, treated, or (in most cases) reversed by diet and lifestyle changes. No drugs required.
So what exactly is insulin resistance (AKA pre-diabetes)?
Insulin is a hormone released by the pancreas. Its primary (though not only) job is to lower the sugar in your bloodstream. It accomplishes this by attaching to the sugar in your bloodstream and escorting it safely into your muscles, where it can be used for energy. When this system works as designed—that is, when the muscles respond to insulin and accept the sugar it offers, you are said to be insulin sensitive, which is a very good thing indeed. Being insulin sensitive is a sign of metabolic health.
Insulin resistance is the opposite of that. It’s what happens in the body when the sugar-removal system stops working as it should. Now the body starts to resist insulin. The muscle cells basically close their doors when insulin comes knocking, saying “we don’t need any more, thank you for asking. Now please go away.”
When the muscle cells start resisting insulin, insulin can no longer “clear” the sugar in your blood stream. The cells just don’t want it. Now you’re left with high blood sugar and high insulin, both of them paddling around the bloodstream like unwanted refugees with no place to dock.
High blood sugar plus high insulin is pretty much the definition of diabetes.
In pre-diabetes, insulin is still somehow, albeit with difficulty, managing to keep your sugar just this side of the number needed for an official diagnosis of “diabetes.” But it’s like a 60s Volkswagen bug trying to keep up on the Autobahn. Make no mistake, it’s only a matter of time before your doctor officially diagnoses you with the dreaded “D” word.
And make no mistake about this as well: Diabetes is pre-heart disease. High blood sugar damages the nerves and blood vessels that control the heart. According to a review in Diabetes Spectrum—a publication of the American Diabetes Association—80% of diabetics die from cardiovascular disease (8). Do the math.
Which is where monitoring your blood sugar comes in.
The more your blood sugar rises, the quicker it spikes, the longer it stays elevated, and the more frequently this keeps happening, the more insulin the pancreas has to release in a frantic attempt to keep blood sugar in a healthy range.
Eventually it can’t and the whole system breaks down.
You want your blood sugar readings to be like the surface of a lake with small gentle waves—you don’t want blood sugar to behave like the Atlantic Ocean during Hurricane Irma.
Which leads us to the obvious question: What raises blood sugar in the first place?
Well, let’s see.
Of the three macronutrients—carbs, fats, and protein—carbohydrates raise blood sugar the most, and have the most profound and dramatic effect on it. Fibrous vegetables (like broccoli) have a smaller effect than, say, rice, but carbs in general affect blood sugar the most, and processed carbs—breads, pastas, cereals, baked goods, cookies and candy—are by far the worst offenders. Eat a plate of beans on Tuesday morning and your blood sugar rises by Wednesday afternoon, but drink 16 ounces of apple juice or a “healthy smoothie” made with fruit, yogurt and juice, and your blood sugar will rise like the Challenger in mere minutes.
Protein can raise blood sugar—since some protein can convert to sugar through a process called gluconeogenesis—but protein doesn’t begin to impact blood sugar nearly as much as carbs do.
And fat? Well, fat doesn’t even move the needle.
Once you understand this eye-opening fact about dietary fat you begin to fully appreciate the insanity of recommending a high-carb low-fat diet to people struggling with weight and diabetes. High-carb low-fat diets are precisely what you don’t need. They will drive blood sugar and insulin through the roof, exactly the opposite of what you want when you’re battling weight gain and trying to prevent diabetes. Remember, insulin’s nickname is “the fat-storing hormone,” and that’s not by accident.
My 5-Step Plan for Reversing, Treating, or Preventing Insulin Resistance
My five-step plan for preventing, treating, or even reversing insulin resistance is simple.- Change your diet. The most likely culprits in your diet—by which I mean the foods most likely to have put weight on you in the first place and most likely to eventually cause insulin resistance—are the processed carbs like breads, pasta, baked goods of all kinds. The more you can cut these out, the better. It’s true that you can reverse insulin resistance with a number of different dietary strategies, but in my experience the strategy with the most likelihood of succeeding is a low-carb diet with plenty of good fat and moderate amounts of protein.
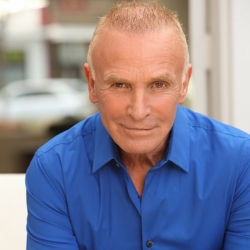
- Learn to fast. Intermittent fasting has been shown in peer-reviewed literature to reduce insulin resistance (9). In addition, fasting helps you lose weight and detoxify as well. It’s also been shown to lower the risk for chronic diseases (10). If you’re interested in intermittent fasting but don’t know where to start or how, I have a video course to get you started. It’s called The 5-Day Intro to Intermittent Fasting and you can download it for free on the home page of my website, www.jonnybowden.com.
- Exercise every day. It doesn’t have to be extreme, just enough movement to create a demand for fuel by the muscle cells. A daily walk is a great idea. Bonus points if you do it after dinner!
- Supplement for basics. Supplements will not reverse or treat insulin resistance, but they will insure that you’re not nutrient deficient and that your metabolism has the nutrients it needs to run smoothly. Remember, when the fat cells begin to empty—i.e. when you’re “burning” fat—a lot of toxins can be released into the bloodstream. Those toxins have to be detoxified and removed (by the liver’s cytochrome P450 enzyme system) and the proper operation of that system is completely dependent on specific nutrients. Supplementing with the basics is a good way to insure that you don’t come up short. I recommend four basic supplements for just about all my clients: a high-quality multiple, fish oil, magnesium, and vitamin D. This protocol will give you the biggest return on investment for the fewest number of pills.
- Improve sleep and reduce stress. Sleep and stress are two of the biggest influences on metabolism and the two of them intimately connected. When you don’t sleep long enough, soundly enough, or deeply enough, the body sees that as a major stressor and releases the same hormone that it releases when you’re stuck in traffic and late for a meeting: cortisol. Cortisol is a great hormone and is essential for emergencies. It’s exactly what you want if you need to run from a bear or fight off a saber-tooth tiger, which is why it’s always been known as the “fight or flight” hormone. But cortisol is a bit like first gear on a car—great for short bursts of activity like getting out of a ditch, but terrible for cruising down the 405 freeway at 70 mph. Our stressed out, sleep-deprived lives keeps the cortisol machinery constantly “on.” Because cortisol is an “emergency” hormone that responds to stress by getting you ready to either fight or flee, it creates glucose (sugar) so that your muscles will have more fuel to run or fight with. The surge of emergency glucose created by cortisol can drive your insulin up almost as much as a high-carb meal. If this happens frequently, you can create insulin resistance even if you’re not eating a lot of carbs. Moral of the story: Find a way to reduce and manage stress, and find a way to improve your sleep. If you want to defeat insulin resistance, then stress reduction and sleep improvement are both critical. Meditation, deep breathing exercises, apps like Calm, exposure to sunlight, and unhurried walks are all great ways to start.
Excess weight, pre-diabetes, elevated blood sugar and high levels of stress are just the late markers of metabolic dysfunction. Change a few basic parameters of your lifestyle—like cutting back on processed foods and introducing intermittent fasting—and you will be on your way to metabolic health.
That’s how you get rid of pre-diabetes.
It’s also how you prevent it from turning into anything worse.
REFERENCES
- https://www.unc.edu/posts/2018/11/28/only-12-percent-of-american-adults-are-metabolically-healthy-carolina-study-finds/
- https://emedicine.medscape.com/article/122501-overview
- https://diabesity.ejournals.ca/index.php/diabesity/article/viewFile/19/61
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8031259/#:~:text=without%20diabetes%20mellitus.-,COVID%2D19%20triggers%20insulin%20resistance%20in%20patients%2C%20causing%20chronic%20metabolic,than%20those%20without%20diabetes%20mellitus.
- https://www.frontiersin.org/articles/10.3389/fpubh.2020.00184/full
- https://www.wjgnet.com/1948-9358/full/v12/i9/1550.htm
- https://www.amazon.com/Great-Cholesterol-Revised-Expanded-Disease-ebook/dp/B08LPHRYVX/ref=sr_1_3?crid=2KEO9V30MYIA0&keywords=great+cholesterol+myth+revised&qid=1640138005&sprefix=great+cholesterol+myth+revised%2Caps%2C136&sr=8-3
- https://diabetesjournals.org/spectrum/article/21/3/177/2020/Best-Practices-for-Lowering-the-Risk-of
- https://clindiabetesendo.biomedcentral.com/articles/10.1186/s40842-020-00116-1
- https://pubmed.ncbi.nlm.nih.gov/27810402/