Let’s start with high blood pressure, or the more formally known “hypertension.” New guidelines from the American Heart Association and the American College of Cardiology lower the definition of high blood pressure to 130/80 millimeters of mercury or greater from the previous 140/90.
The new recommendation stems from the results of a federally-funded study published in The New England Journal of Medicine. Under the new guidelines, the number of American adults with high blood pressure will rise from 72 million to 103 million and an estimated 4.2 million will be candidates for high blood pressure medication.
“We want to optimize people even more,” says Dr. Michael Smith, MD, senior health scientist, LifeExtension, Fort Lauderdale, FL, about the new guidelines. “Believe it or not, we target 115/75. That’s where you have the lowest incidence of cardiovascular consequence.”
Laurel Sterling, MA, RD, CD/N, nutritionist and educator with Carlson Laboratories, Arlington Heights, IL, says it’s always best to look at lifestyle factors first before turning to medication. She suggests looking at more sensitive testing procedures (C-reactive protein for inflammation, fibrinogen, etc.).
The most effective ingredients to support healthy blood pressure, she says, are omega-3s, coenzymeQ10, magnesium, vitamin E, garlic, amino acids (l-arginine, l-carnitine, l-taurine, l-citruline).
A 1994 study published in theJournal of Hypertensionconcluded that krill oil can assist in controlling high blood pressure when taken in addition to implementing a healthy lifestyle. It found a greater reduction in the level of blood pressure and plasma triglycerides by omega-3 fatty acids from krill oil in treated hypertensives as an adjunct therapy to beta-blockers or diuretics. The blood pressure levels were significantly lower in the krill oil group than in the patients taking beta-blockers or diuretics alone.
The World Health Organization estimates that hypertension is the most common chronic condition worldwide, affecting 1 billion people and accounting for one in eight deaths each year.
“When you put pressure on the artery, the artery must be able to compensate. If the artery is very stiff, the pressure will build up. Hypertension is not good on cardio or vascular, and kicks back on all the other organs, causing them not to function properly,” says Barrie Tan, Ph.D., founder of American River Nutrition, Hadley, MA. American River produces Delta Gold, a patented vitamin E that contains the natural ingredient tocotrienol from the annatto plant.
An open label study published in the British Journal of Medicine and Medical Research indicates the optimal dose of tocotrienol is 250 mg/day to lower total cholesterol, LDL, triglycerides and cytokines associated with cardiovascular disease (1).
“For tocotrienol and hypertension, in animal studies, we consistently found that the blood pressure dropped,” Tan says. “Because of the new recommendations, a future clinical study on tocotrienol may specifically include an end point for hypertension to see if the consistent findings we noted in animal studies translate to human studies. For now, the preclinical animal studies are compelling enough to support arterial protection by tocotrienol.”
The Role of Healthy EatingThe DASH (short for Dietary Approaches to Stop Hypertension) Diet, which was developed by the National Institutes of Health, ranked No. 1 for “healthy eating” and “heart disease prevention” among nearly 40 diets reviewed recently by U.S. News and World Report. The low-sodium diet has the potential to lower blood pressure as well as or better than many anti-hypertension medications.
The diet focuses on vegetables, fruits, whole grains, low-fat dairy, lean proteins, beans and nuts. It is rich in potassium, calcium and magnesium along with protein and fiber. DASH requires a reduction in high-fat red meat, sweets and sugary beverages.
Researchers funded by NIH’s National Heart, Lung and Blood Institute (NHLBI) developed DASH to prevent and treat high blood pressure, but the diet also has proven effective in lowering blood cholesterol. Positive effects have been recorded in two weeks. Over time, the systolic blood pressure (top number) could drop by eight to 14 points.
When DASH is combined with low-sodium intake, a new study shows adults with stage one prehypertension were able to “substantially lower” systolic blood pressure (2), says Janet de Jesus, M.S., registered dietitian and program officer at NHLBI’s Center for Translation Research and Implementation Science.
“The effects are greater in people with hypertension or higher blood pressure at baseline, which is comparable to anti-hypertensive medications,” adds Stephen Juraschek, M.D., an instructor of medicine at Harvard Medical School and the study’s first author. “Our results add to the evidence that dietary interventions can be as effective as — or more effective than —antihypertensive drugs in those at highest risk for high blood pressure, and should be a routine first-line treatment option for such individuals.”
When it comes to eating well, choosing certain culinary oils can play a big role. Among Carlson’s products are Omega-3 infused finishing oils that can be used, for instance, when making hummus or drizzling over a salad. Olive oil and the Mediterranean diet have been long known to assist with cardiovascular health because of the monosaturates and omega-9, Sterling says.
Not many people get the heart healthy omega-3s and omega-9s in one combination, she adds. The extra-virgin olive oil also has polyphenols. “That’s the root cause of a lot of diseases now,” Sterling says. “Teaming that with the omega-3s, we thought was a great no-brainer combination. There are more than 30,000 different studies on omega-3s and the rate of positive findings in clinical trials is consistently high. We base a lot of our product formulation on current research.”
She adds that as for the omega-6s, flax oils and seed oils from the omega-6s would be beneficial. Omega-6s are too prevalent in our diets compared to our omega-3 consumption. This disproportion plays a big role in our failing health. Therefore avoid processed and fast food, consume a good deal of omega-3s and get omega-6 from healthy sources.
Doctors recommend reducing sodium intake to 1,500 mg a day for those who have hypertension or are at high risk of developing hypertension. Risk increases after age 50. Another lifestyle change to maintain healthy blood pressure is weight management. For overweight people, blood pressure can drop by one point for every 2.2 pounds of weight lost. Aerobic exercise for 90 to 150 minutes per week can lower blood pressure five to eight points.
“Homeopathy addresses heart health in ways that lifestyle and nutrition alone cannot,” says Dr. Frank King, founder of Dr. King’s by King Bio, Asheville, NC. “Herbs and nutrition work on the biochemical (literally ‘life chemical’) level. Homeopathy works on a bioenergetics (‘life energy’) level, much like chiropractic and acupuncture treatments help open the nerve energy flows of the body.“
Homeopathic medicine, he adds, can help with inherited genetic predispositions for weak heart function, weak arteries, irregular pulse, high cholesterol, or poor circulation, and recommends homeopathically prepared Digitalis (foxglove) and nitroglycerine as safe ways to support heart health.
Deep breathing, meditation, yoga, and other relaxation techniques may also help to reduce blood pressure and stress level. What you consumed or did immediately before your blood pressure was taken can cause an unusual spike. Sit for awhile and ask for a second reading if your blood pressure registers as elevated.
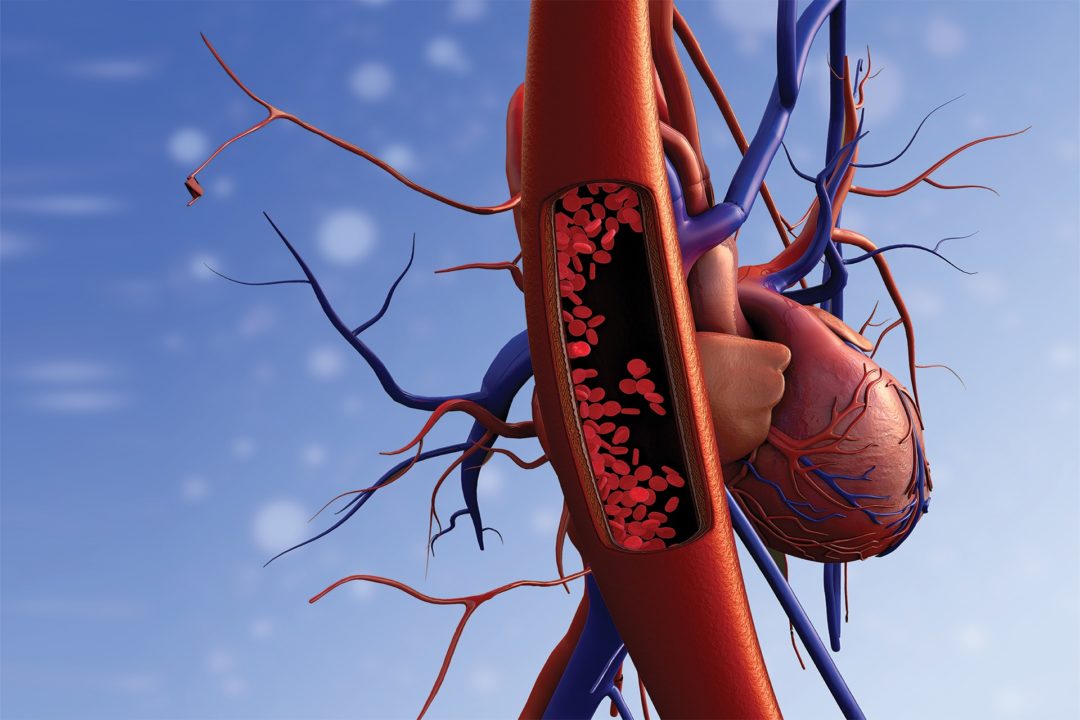
Inflammation“In the human body, there are 36,000 miles of arteries,” Tan notes. “The pressure is pushed into the artery and relieved in the vein. So now when the cardiovascular system pumps the blood it has to go 36,000 miles. The center of the cardiovascular system is the heart, and it is similar to a car engine. If the engine doesn’t work, the car won’t. On the other hand, if the car engine works but the other parts are damaged, it’s no good either.
“Today we know that cholesterol is not the only problem,” says Tan. “In the 1990s, research was showing that half of people with cardiovascular events had normal cholesterol. Paul Ridker spent 20 to 30 years at Harvard Medical School to find out why these patients with normal cholesterol levels still had cardiac events. Then he found out the other half of the reason: inflammation.”
Omega-3 EPA/DHA found in fish oils are effective support. “Most fish oil formulas will have more EPA because of its systemic effects. The main things we like to talk about in terms of heart disease and fish oil is really focusing on the ability of the EPA to lower chronic systemic inflammation,” says Smith. “If we can control systemic inflammation, we’ll lower inflammation in the arterial wall.”
Life Extension’s Clearly EPA/DHA concentrated Omega-3 fish oil softgels have 1,500 mg of EPA (eicosapentaenoic acid) for every 1,000 mg of DHA (docosahexaenoic acid). “EPA won’t target a plaque that’s already there, but it will control the original insult to the artery, which is inflammation,” Smith adds. “When you have atherosclerosis, there’s always some insult/injury to the artery. Low-grade inflammation is the constant insult to the thin lining. We really focus on controlling the inflammation that creates plaque.”
“Plaque contains three major things,” says Tan. “Cholesterol, or oxidized cholesterol, fat and oxidized fat, and calcium (approximately one third of each). I think the FDA/RDA of most essential nutrients are low. Except for calcium. I think it’s too high. I ask my wife to take calcium, but I don’t know where the calcium is landing. It doesn’t just land in the bone. I think most of the time it’s landing on the artery. That’s not a good place.”
For that reason, it’s recommended that calcium-takers supplement with vitamin K2, which inhibits arterial calcification and stiffening by preventing the calcium from building up in arteries. Vitamin K2 is known to activate matrix GLA protein (MGP), which inhibits the deposits of calcium on the walls. Little Vitamin K2 is consumed in a Western diet, even a healthy one.
CoQ10 and the Heart“Coenzyme Q10 is a great cardio supplement. It works really well in the heart. I started taking CoQ10 30 years ago,” Tan says. Most CoQ10 is found in animals, but vegan or vegetarians can find it in spinach, broccoli and cauliflower.
It’s especially important for those who take statins to accompany it with CoQ10, Tan explains.
Statins are 3-hydroxy-3-methylglutaryl coenzyme A reductase (HMG-CoA reductase) inhibitors that block internal biosynthesis of cholesterol and its use is an established strategy to lower levels of low-density lipoprotein cholesterol (LDL-C). However, they are an indiscriminate cholesterol reducer.
“Statins block cholesterol biosynthesis which occurs in a metabolic branch known as the Mevalonate Pathway [but] also interfere with production of CoQ10 (ubiquinone and ubiquinol) and other metabolic products,” says Sid Shastri, product development manager for Kaneka Nutrients, Pasadena, TX. “In the simplest of terms, a negative consequence of statins is the depletion of beneficial CoQ10 in the body.
“CoQ10 in the form of ubiquinol (the active form of CoQ10) is the main electron carrier in the mitochondrial electron transport chain so its importance in the role of cellular energy production can impact not only the heart but also all biological processes requiring energy,” Shastri continues.
Kaneka’s ubiquinol was used in a recent study by researchers at the Center for Human Drug Research in The Netherlands. The randomized, double-blind, parallel, placebo-controlled trial aimed to investigate the mitochondrial dysfunction caused by simvastatin treatment (40 mg per day) and determine if ubiquinol could offer a protective effect. According to the study, it can partially reversed mitochondrial dysfunction caused by a statin (6).
“Evidence is growing that the dysfunctional mitochondria play a central role in heart disease and other conditions including neurodegenerative disease, sarcopenia, and type 2 diabetes,” Shastri adds. “The heart’s unending requirement for consistent cellular energy requires that mitochondrial respiratory pathways — where ubiquitol plays a central role — produce adequate energy in the form of ATP.”
One theory explaining the effectiveness of CoQ10 on blood pressure concerns its role as an antioxidant, says Trisha Sugarek MacDonald, BS, MS, senior director of research & development/national educator for Bluebonnet Nutrition, Sugar Land, TX.
“Studies of diabetics have found that increased oxidative stress may underlie endothelial dysfunction by decreasing production and increasing consumption of nitric oxide, as well as generating free radicals,” she says. “CoQ10 has been found to mitigate this effect by reducing oxidative stress. It makes cells healthier and less vulnerable to constriction, thus reducing the pressure inside blood vessels.”
Smith suggests corsitin, melatonin, olive leaf extract, and then fish oil in ranking for added supports among those who are at risk for hypertension. “Fish oils help excitable nerves signal better and regulate how charged particles move through cells. You’ll be seeing more research on using omega-3s for heart arrhythmia and other disorders.”
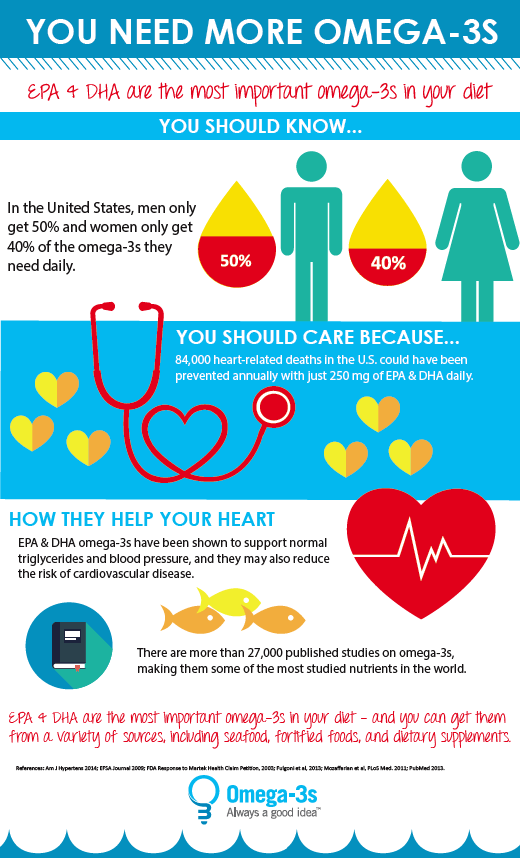
The Omega-3 IndexThe Omega-3 Index reflects the relative amount of EPA + DHA in red blood cells. It is expressed as the percentage of the total amount of fatty acids present. In fact it’s quite simple; if 8% of all the fatty acids present in red cell membranes is EPA+DHA, the Omega-3 Index is 8%. It has been hypothesized that the Omega-3 Index may predict the risk of future cardiovascular events such as coronary heart disease and cardiac arrest. If that’s correct, a low Omega-3 Index may be regarded as a risk factor, similar to smoking, high blood pressure and high blood levels of LDL cholesterol. Recently, a low level of long-chain omega-3 fatty acids had been proposed as a risk factor for heart disease. An omega-3 index of >8% is associated with 90% less risk for sudden cardiac death, as compared to an omega-3 index of <4% (4).
The average Omega-3 Index in the United States is believed to be between 4-5 %. In Japan, where coronary artery disease is less common and life span longer, the average Omega-3 Index is 9-10%. (5)
In the Physicians’ Health Study, healthy men were followed for up to 17 years. The fatty-acid composition of previously collected blood was analyzed for 94 men in whom sudden death occurred as the first manifestation of cardiovascular disease and for 184 controls matched with them for age and smoking status.
Compared with men whose blood levels of long-chain omega-3 fatty acids were in the lowest quartile, the relative risk of sudden death was significantly 70% lower among men with levels in the third quartile and 80% lower in the fourth (highest) quartile. The levels of omega-3 fatty acids are strongly associated with a reduced risk of sudden death among men without evidence of prior cardiovascular disease (5).
“There’s a lot of violent heart attack issues with men and women starting in their 40s,” says Sterling. “That may be hurting them when they try to get life insurance, etc. If they have a risk factor with that involving diabetes or a history in the family of heart attack and stroke, they need to look at all of those in total. Depending on where all this is coming from, on the one hand it’s better they’re flagged sooner. Hopefully they’ll be treating lifestyle factors first,” says Sterling, noting concentrated doses of fish oil omega-3s can be helpful.
The Omega-3 index looks at the amount of DHA and EHA in blood cell endings. Omega-3 testing is not one that’s been a standard test done in the doctor’s office, so it has to specifically requested.
The Institutes of Medicine has not established a recommended intake level for omega-3s, but the Global Organization of EPA and DHA Omega-3s (GOED), has gathered research and recommendations from health authorities around the world and has come up with a benchmark of 500 mg combined EPA and DHA per day per adult.
Researcher William Harris, MD, believes that is far too low to move the needle in terms of this risk factor. He says boosting individual consumers’ Omega-3 Index could be just as important as managing other ‘silent’ risk factors, such as high blood pressure.
“It’s much like vitamin D testing, you can’t feel a low omega-3 level. You can’t feel high cholesterol. Without some test you can’t know if you need to take omega-3s. Even people who say they eat a lot of fish, they may be eating fried catfish and shrimp, which have very low omega-3s,” Harris says. “From the data we’ve got from dose response studies we’ve done, it’s going to take about 1.5 g of EPA and DHA combined to get them up to that 8% level.”
Adam Ismail, executive director, GOED, Salt Lake City, UT, is bracing for a lot of media focus on omega-3 this year because of some big upcoming research reports that could go one way or the other.
“The biggest events will be the publication of the VITAL and REDUCE-IT studies, which will be two of the largest omega-3 clinical trials ever published. I personally have concerns that the VITAL study will show a reduced risk of coronary deaths, but that it will not reach statistical significance.
“Most of the trials published to date have shown approximately 10% reductions in relative risk of CHD (coronary heart disease) mortality, but the VITAL study was powered to detect a much larger effect, which means fewer subjects would be needed. However, there are still reasons to be optimistic. For one, most of the trials published to date have been in populations that were already being treated for heart disease, but the VITAL study is a primary prevention trial.” explains Ismail.
Other recent meta-analyses, he says, have observed bigger events when there are fewer subjects on statin drugs but with high cholesterol or triglycerides; much closer to the population that VITAL will be studying. “The fear here is that a non-significant benefit will turn into negative headlines that not only drive consumers away from omega-3 supplementation but also healthy fish consumption, “ he continues.
“The REDUCE-IT trial is studying something similar but in people being treated for aspects of CHD already. Importantly, it is a trial to support Amarin’s Vascepa omega-3 based pharmaceutical, but it will have some important implications beyond just supporting their own product.
“The public health policymakers have yet to be convinced that lowering triglycerides actually impacts one’s risk of CHD, but this study will add important data in this area,” Ismail says.
The CANTOS study earlier this year found that reducing other markers of heart disease — such as inflammation — can reduce CHD risk. While this was not an omega-3 trial, it does take the matter beyond the “dogma” that only blood pressure and LDL cholesterol can impact CHD risk, he adds.
The REDUCE-IT and VITAL studies will bring a lot of media attention to omega-3s in 2018. “It could be positive or negative,” he says, “which means it will definitely be turbulent.”
Krill Oil Benefits
"Krill oil provides the body’s best source of omega-3 essential fatty acids," says Hank Cheatham, VP, marketing and sales, Daiwa Health Development, Gardena, CA. "It is rich in phospholipid EPA and DHA providing greater bio-availability, superior to fish and flax oils, with no 'fishy' aftertaste."
Krill oil is a super antioxidant composed of pure oil derived from Antarctic krill. Krill are plentiful, tiny, bright pink, shrimp-like crustaceans.
Krill oil also contains astaxanthin, a powerful antioxidant as well as the fatty acids omega-6 and omega-9, and vitamins A and E.
Not All Krill Oil Is Alike
"There are some significant differences among krill oils even though all of the oil is harvested from krill," Cheatham adds. "Some unscrupulous suppliers try to market fish oil but label the product krill oil because fish oil is generally much less expensive. Even though both marine oils provide omega-3s, only krill oil contains the antioxidant astaxanthin giving krill oil its unique red/pink color.
"The best quality krill oil," he adds, "is produced with oil that is completely traceable to the exact location in the Antarctic where the oil is harvested and the deep water is pristine, free of heavy metals, toxins and other contaminants that can be found in fish oils. Not only is the purest and most responsibly controlled krill oil sourced from the Antarctic Ocean, but the harvesting is regulated by the Commission for the Conservation of Antarctic Marine Living Resources (CCAMLR).
Krill oils differ in the amounts of omega-3 EPA and DHA they offer as well as the amount of phospholipids and astaxanthin contained in the oil. Daiwa Super Krill Oil is richer in omega-3s, phospholipids, choline and astaxanthin than most other krill oils, Cheatham adds. It uses a technology that removes unwanted salts and other polar constituents while boosting omega-3s (EPA/DHA), phospholipids, astaxanthin and choline.
New Heart Health Research
Coronary inflammation can lead to plaque rupture and blood clot formation in the heart. Several inflammatory markers can indicate the presence of chronic inflammation and risk for cardiovascular disease, i.e. fibrinogen, C-reactive protein (CRP) and interleukin-6 (IL-6). A study by D. J Rader, published in the New England Journal of Medicine, Inflammatory Markers of Coronary Risk, confirms that people who have high levels of fibrinogen are twice as likely to suffer from heart attack as those with normal levels.
The inflammatory response also stimulates production of another marker called CRP. CRP is produced by the liver. Individuals with increased CRP levels have been shown to be three times as likely to have a heart attack as those with normal levels.
Krill Oil can reduce the levels of fibrinogen, CRP and IL-6 in the body naturally, thereby, reducing the probability of heart attack and other myocardial damage. Krill oil’s benefit to the heart is confirmed in a scientific study by L. Deutsch,Evaluation of the Effect of Neptune Krill Oil on Chronic Inflammation and Arthritic Symptoms, published in the Journal of the American College of Nutrition. There is substantial scientific evidence to support krill oil’s significant benefit to heart health.
WF
References