Dr. Hill noted that these are not legally binding papers; they don’t impose anything on anybody—rather, “they’re meant to provide a common language,” because, as he said, “if we don’t have a common language, it’s very difficult to communicate with one another.” The terms are defined as a service to the industry, not a government regulation.
Dr. Hill and his colleagues have a paper in final review on the definition of postbiotics, and he discussed the definition with the public for the first time during his Naturally Informed sessionPostbiotics: What are they and how do they work. He described the process by which experts are convened and the consensus paper is written. He discussed how they landed on the term postbiotics, rather than choosing paraprobiotics, heat-killed probiotics, or any other term that has been used for this concept. He explained that things like bacteriophages, butyrate, and fermentates are excluded—“We made a very early decision that we do not need to define things that already have definitions. If something already has a term, we don’t need to define them or encompass them. A bacteriophage is not a postbiotic, it’s a bacteriophage.”
The final definition:Preparation of inanimate microorganisms and/or their components that confers a health benefit on the host.
Dr. Hill went on to pull the definition apart and explain it, piece by piece, and to explain how postbiotics work, along with several examples. Register atNaturallyInformed.net to watch the full presentation.
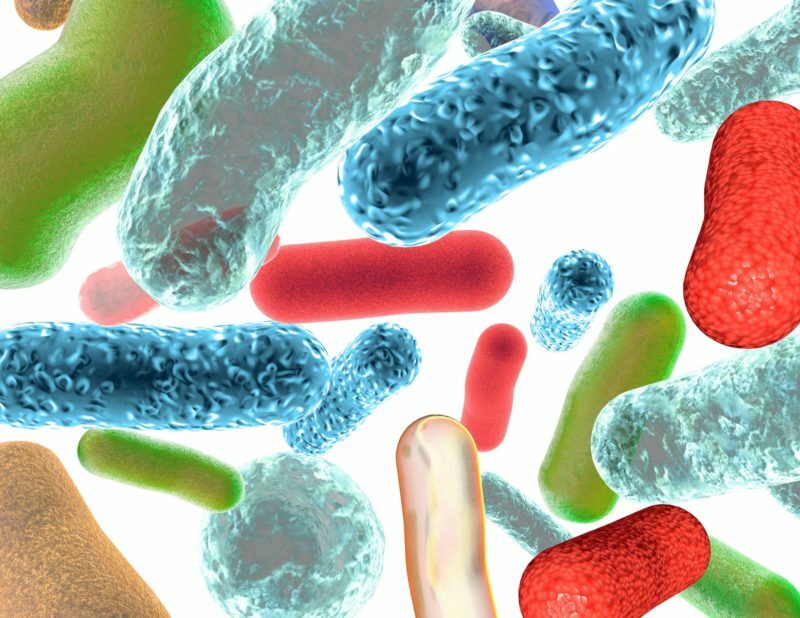
Those interested in the growing sports nutrition segment will be interested in the presentation from Douglas S. Kalman, Ph.D., RD, VP of Scientific Affairs at Nutrasource, who brought data for athletes—and those curious about how working out could affect their microbiomes. As it turns out, exercise, too, confers a health benefit on the host. Dr. Kalman explained that athletes have a different microbiome, affecting their nutrient uptake: “We know that physical activity on its own includes the promotion of a higher abundance of health-promoting bacterial species, increasing the microbial diversity of the gut, which enhances the functional metabolic capacity.” This improves immune function as well as digestive function.
Dr. Kalman discussed the specific differences between sedentary people, “weekend warriors,” and professional athletes—right down to individual strains, such asVeionella atypica—noting that athletes’ microbiomes actually prime their bodies for tissue repair, while helping them harvest energy from calories ingested. He also talked about how certain foods like fats affect the microbiome, and discussed an ongoing study that seeks to determine how different levels of exercise may impact the microbiome. For details, watch his presentationSports, Athletics and the Microbiome—Does it Matter?
Related: #NaturallyInformed: Driving Education in the Microbiome Space When Times Seem Tough, Resilience Keeps You in the Game Consumer Survey Reaffirms Consumer Confidence, Trust in the Industry
And those interested in the ever-popular curcumin will want to view the presentation by Anurag Pande, Ph.D., VP Scientific Affairs at Sabinsa, who walked attendees through a case study on how curcumin can affect the microbiome. Following an in-depth explanation of the human microbiome and how it changes over the course of a lifetime—from gestation to old age—he explained that “curcumin’s health benefits may not be necessarily relying on the bioavailability itself—which has always been a topic to consider—but may actually be resulting from its positive effect on the gut, and its effect on the microbiome itself.”Looking at the data, Dr. Pande pointed to studies that show that bioavailability doesn’t always have a direct effect on the efficacy, and that “curcumin has significant gut effects, as well as systemic effects. Some of the most compelling evidence of [the benefits of] curcuminoids are actually observed in colon health studies.” In a mouse model, Dr. Pande explained, curcumin it reduced colonic tumor burden, and in other studies performed on mice, curcuminoids have been shown to help maintain a diverse and healthy colonic microbiome. When mice are fed a high-fat diet but supplemented with curcumin, their microbiome shifts towards the microbiome seen in mice on a lean diet.
Dr. Pande also discussed a double-blind, randomized, placebo-controlled clinical trial using Sabinsa’s C3 Complex, which found that the curcumin had “prebiotic-like” effects that were helpful for the growth of beneficial GI bacteria, increasingBacteroidetesin the subjects. Curcumin, too, as it turns out, can confer a health benefit on the host. For the details, and to find out how much C3 Complex altered the microbiome compared to turmeric and to placebo, check out his presentationCase Study: Curcumin and Microbiome Modulation.
James LaValle, Clinical R.Ph., CCN, MT, N.D., discussed the connection between the gut, immunity, and the brain, and the things that can disrupt that connection. One issue he sees in his practice: The rising prevalence of food sensitivity. He explained that this is in part due to how the immune system functions, beginning with sensitization—“If you don’t have enough adequate beneficial flora, and you’re not making enough butyrate, you can’t keep the tight junctions between the mucosal cells. There’s only one cell layer between your mucosal cells and things being able to enter your bloodstream.” Much in the same way that inhaling a cold germ leads the immune system to produce antibodies, allowing the immune system to mount a response the next time the cold germ enters the body, allergens that slip through the mucosal cell lead to the production of antibodies—and to a heightened immune response. And those allergens aren’t always pathogens, Dr. LaValle said—they can be things like dairy or gluten. The results, he says, could lead to everything from rashes to depression.
Over the course of the rest of Dr. LaValle’s presentation, he discussed inflammatory aging, food cravings, anxiety, IBS, stress, and more—and the connection between that whole list and the gut. He also discussed drugs that are known to affect the microbiome, ranging from OTC drugs to opioids, and probiotics that can help. The whole presentation,Gut—Immune—Brain Connection: The Importance of Prebiotics and Probiotics to Maintain Resilience, as well as every presentation from this conference, is available on demand atNaturallyInformed.net.