I called upon vitamin K researcher, Dr. Leon Schurgers. Dr. Schurgers was kind enough to share his thoughts on the functions of vitamin K, discuss the significance of new research findings and comment on the potential implications for clinical practice for us. Since February is Heart Month, we will focus largely on the cardiovascular system, but also discuss skeletal health.

Dr. Stephen Sinatra greatly increased my interest in vitamin K2 during our recent series of interviews. When Dr. Sinatra mentioned in our June 2007 chat that vitamin K2—but not vitamin K1—could reduce harmful calcium deposits from arteries, that was it. I had to learn even more. When I read the research reports of Dr. Leon Schurgers and saw his dramatic illustration of the effect of vitamin K2 on arterial calcification (Figure 1), I knew this was indeed an important breakthrough in treating cardiovascular disease. So, I called upon vitamin K researcher, Dr. Leon Schurgers. Dr. Schurgers was kind enough to share his thoughts on the functions of vitamin K, discuss the significance of new research findings and comment on the potential implications for clinical practice for us. Since February is Heart Month, we will focus largely on the cardiovascular system, but also discuss skeletal health.
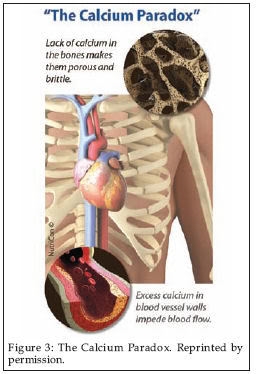
We will discuss the “calcium paradox,” by which so many people are having harmful calcium deposits form in their arteries at the same time that calcium content of the bones is decreasing. This calcium paradox is not a result of too little calcium in the diet, but of too little vitamin K2 that largely controls where the calcium goes. The objective is to keep calcium in our bones, not in our arteries. This is the role of vitamin K—putting calcium in its place!
 As most of our readers know, but few in the general public know, the amount of calcium that circulates in the blood is rigorously under hormonal regulation. The amount of calcium in the blood is critical to such functions as the heart beat, muscle contraction, vasodilatation and nerve transmission so the level of calcium is under hormonal regulation. If the diet is low in calcium, the parathyroid hormone will increase the blood level of calcium by facilitating calcium removal from the skeletal tissues. Our readers understand that bone is active, dynamic, living tissue, not calcium chalk.
As most of our readers know, but few in the general public know, the amount of calcium that circulates in the blood is rigorously under hormonal regulation. The amount of calcium in the blood is critical to such functions as the heart beat, muscle contraction, vasodilatation and nerve transmission so the level of calcium is under hormonal regulation. If the diet is low in calcium, the parathyroid hormone will increase the blood level of calcium by facilitating calcium removal from the skeletal tissues. Our readers understand that bone is active, dynamic, living tissue, not calcium chalk.
On the other hand, calcitonin (a hormone produced by the parafollicaular cells [C cells] of the thyroid gland) acts to decrease calcium concentration when levels are high.
 Vitamin K functions as a coenzyme during the activation of a number of proteins involved in blood coagulation, bone formation and keeping blood vessels free of calcium. This “activation” is achieved by vitamin K assisting the production of a “carboxylated” form of these proteins.
Vitamin K functions as a coenzyme during the activation of a number of proteins involved in blood coagulation, bone formation and keeping blood vessels free of calcium. This “activation” is achieved by vitamin K assisting the production of a “carboxylated” form of these proteins.
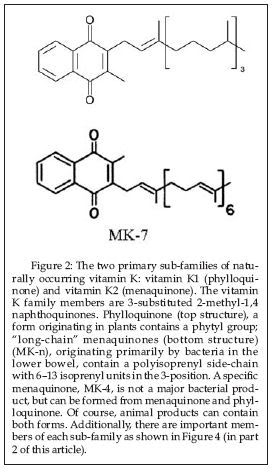
Vitamin K has been known as the “coagulation vitamin” since its discovery, which is usually credited to the Danish scientist, Dr. Henrik Dam in 1929. The letter “K” used to designate the vitamin is from the German word Koagulationsvitamin. Through the years, it has been found that vitamin K is not a single compound, but a family of compounds having similar chemical structural features. There are two main sub-families within the vitamin K family.
Within the past three decades, the essential role of K vitamins in maintaining bone and cardiovascular health has become known as a significant amount of research has published. Not only do the K vitamins play an important role in forming blood clotting proteins in the liver, the K vitamins are required for the proper functioning of the proteins such as the three bone-mineralizing proteins (especially the Gla-protein osteocalcin) and the widely distributed calcification-inhibiting matrix Gla protein (MGP) that keeps calcium out of arteries.
It is especially important to note that Western populations are vitamin K-deficient for optimal bone and heart health. Even if people consume sufficient vitamin K to ensure proper blood clotting, larger amounts are necessary to sustain bone and blood vessel health, particularly in aging adults. It is also interesting to note that much of the vitamin K research is done by groups in the Netherlands, where the population consumes a diet considerably higher in vitamin K than the U.S. population.
Dr. Leon Schurgers is a senior scientist in biochemistry at the Maastricht University in The Netherlands. He is vice president for VitaK Research at the Maastricht University, the world’s largest research institute dedicated to vitamin K. Furthermore, as a senior scientist for the Division on Vitamin K Research, Dr. Schurgers is part of the Cardiovascular Research Institute, the largest research institute of the University of Maastricht. Dr. Schurgers’ major occupation is leading the scientific part on vitamin K research and supervising technical engineers, post-docs and Ph.D. students. Dr. Schurgers is a member of the American Society of Bone and Mineral Research, the International Society on Thrombosis and Haemostasis as well as the American Heart Association. He has published over 50 research papers in the international scientific press.
Passwater: What led you to become a biochemist?
Schurgers: As a child I had many questions, always related to “how” and “why.” I guess my scientific instinct was already present at a young age. Also, during my education, the human body and how life develops, works and sometimes fails always fascinated me. I find it continuously fascinating and very satisfying intellectually. Biochemistry is the “Chemistry of Life,” where we are able to take advantage of recent progress in knowledge and to translate them into health benefits and solutions. Being central to all sciences, biochemistry gives us the opportunity to utilize this knowledge for the benefit of all.
Passwater: Why did you research vitamin K? After all, until now, it hasn’t been a sexy vitamin to study.
Schurgers: When I started my career at the Maastricht University, our group was part of the Cardiovascular Research Institute Maastricht (CARIM). Thus, we all worked on vascular disease. My interest was focused on MGP, a vitamin K-dependent inhibitor of arterial calcification. It intrigued me that this inhibitor could be modulated: its activity depends upon vitamin K! At first sight, nobody was interested in calcification, as it was regarded as a passive process, always present in diseased arteries. It was not thought to be of clinical importance then. Now, calcification is regarded as one of the most predictive values of vascular disease, and vitamin K plays a major role.
 Passwater: We’ll get back to the role of MGP later. How did vitamin K2 get into your research picture?
Passwater: We’ll get back to the role of MGP later. How did vitamin K2 get into your research picture?
Schurgers: As two natural sub-families of vitamin K are known, designated as K1 (phylloquinone) and K2 (menaquinone), they needed further evaluation. Because of their dissimilarity in chemical structure, these two sub-families of vitamin K have different bioactivities, efficacies and bioavailabilities, which impact the way they function within the body. Figure 2 shows the chemical structures of the two vitamin K sub-families.
During my Ph.D. process I studied the bioavailability and bioactivity of each form. We found that vitamin K1 goes primarily to the liver, and only a small amount is released for the periphery, whereas vitamin K2 is equally distributed over our body, via the redistribution in the liver in VLDL and LDL particles via the blood. Therefore, vitamin K2 can be of great importance for peripheral tissues such as the arterial vessel wall.
Passwater: Very interesting. Please elaborate more on why our readers should care about vitamin K2.
 Schurgers: While K1 is poorly absorbed and has little influence on cardiovascular health, K2 has a beneficial effect on both bones and vasculature. In the nutritional (physiological) dosage range, natural vitamin K2 provides the source of vitamin K preferred by extrahepatic tissues, including bone, cartilage and soft tissues. Vitamin K2 prevents arterial calcium accumulation, which is associated with the development of cardiovascular disorders. I believe our research is having a very good impact on vitamin K usage in general, which is particularly important when vast the vitamin K deficiency in the Western population is taken under consideration.
Schurgers: While K1 is poorly absorbed and has little influence on cardiovascular health, K2 has a beneficial effect on both bones and vasculature. In the nutritional (physiological) dosage range, natural vitamin K2 provides the source of vitamin K preferred by extrahepatic tissues, including bone, cartilage and soft tissues. Vitamin K2 prevents arterial calcium accumulation, which is associated with the development of cardiovascular disorders. I believe our research is having a very good impact on vitamin K usage in general, which is particularly important when vast the vitamin K deficiency in the Western population is taken under consideration.
Passwater: Keeping calcium out of our arteries and in our bones certainly is a great take-home message. The need for K2 in keeping calcium in bones seems straightforward, but how did you elucidate the fact that vitamin K2 can remove calcium from arteries?
Schurgers: We have shown that cardiovascular disease and osteoporosis have some common pathways and elements. Studies carried out during the last decades showed that calcium can be definitively linked to the two diseases. In laymen’s terms, this is put forward as the “Calcium Paradox” (see Figure 3): while lack of mineral in the bones makes them weak, excessive amounts of calcium in blood vessels makes them more rigid, leading to hypertension and subsequently cardiovascular disease.
The first clues that vitamin K2 is important for cardiovascular health came from the so-called “Rotterdam Study.” In this prospective study, healthy elderly people consuming the highest intake of dietary vitamin K2 had some 50% less vascular calcification and cardiovascular death. Thus, the link between vitamin K2 consumption and vascular disease was established. This work has now been confirmed by a second, independent study showing the same trend.
Passwater: Does this apply to reversing calcium accumulation in the arteries as well as halting further accumulation of calcium in arteries over time?
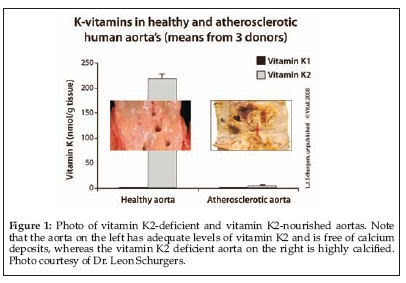 Schurgers: Yes indeed! At least that’s the hypothesis we put forward. The Rotterdam Study gave us the clue for in which direction to look. We found out that MGP acts as a strong inhibitor of vascular calcification. MGP was shown to be the strongest inhibitor of arterial calcification, which fully depends for its functionality on vitamin K. We have tested this in experimental animals and it was shown that vitamin K2 could fully protect against warfarin-induced arterial calcification and even could reduce existing vascular calcification by 37%.
Schurgers: Yes indeed! At least that’s the hypothesis we put forward. The Rotterdam Study gave us the clue for in which direction to look. We found out that MGP acts as a strong inhibitor of vascular calcification. MGP was shown to be the strongest inhibitor of arterial calcification, which fully depends for its functionality on vitamin K. We have tested this in experimental animals and it was shown that vitamin K2 could fully protect against warfarin-induced arterial calcification and even could reduce existing vascular calcification by 37%.
These latest findings on the importance of vitamin K2 intake may mean a major advance for the treatment of cardiovascular diseases, as our experiments gave evidence that vitamin K2 supplementation is capable of not only stopping, but also reversing the effects of arterial calcification. Before any conclusions can be drawn for humans, we need to study this effect in human clinical trials. However, the results thus far look very promising.
Passwater: We’ll discuss the importance of the warfarin-vitamin K antagonism shortly, but I want to clear up one thing. Are these all animal studies or is there human clinical evidence as well?
 Schurgers: The benefits of vitamin K2 on blocking and regressing calcification are indeed animal studies. However, a benefit of vitamin K2 for prevention of cardiovascular disease was shown in the Rotterdam Study. The Rotterdam Study, involving approximately 4,800 people over a 10-year period, revealed that increased dietary intake of specifically vitamin K2 significantly reduced the risk of CHD mortality by 50% as compared to low dietary vitamin K2 intake.
Schurgers: The benefits of vitamin K2 on blocking and regressing calcification are indeed animal studies. However, a benefit of vitamin K2 for prevention of cardiovascular disease was shown in the Rotterdam Study. The Rotterdam Study, involving approximately 4,800 people over a 10-year period, revealed that increased dietary intake of specifically vitamin K2 significantly reduced the risk of CHD mortality by 50% as compared to low dietary vitamin K2 intake.
What is more, outcomes of some new studies revealed that patients on hemodialysis (kidney disease) are typified by low protection against arterial calcification due to poor vitamin K status. Also, patients suffering from cardiovascular disease such as aortic stenosis and heart failure showed a poor vitamin K status. In the first pilot results, supplementing dialysis patients with vitamin K2, clearly show a significant benefit of vitamin K2 as menaquinone-7 (Mk-7). If this will lead to less calcification and eventually less death, it needs to be investigated.
I emphasize that the calcification of the arteries seen in chronic kidney disease is the same type of calcification that is found in aging population. The accumulation of calcium in the arteries results in stiffening and increased fragility. This might be considered a silent killer, as hardening of the arteries develops without any symptoms over time. The process of calcification is an actively regulated process and that adequate vitamin K2 intake can prevent this process and potentially reduce this risk factor.
 Passwater: Let’s give our readers a break here and come back next month in Part 2 with a discussion of the research showing that nutritional levels of vitamin K2 can reverse calcium deposits in arteries, the effect of vitamin K2 on bone health. Also covered will be how vitamin K works in the body, what are adequate and optimal levels of vitamin K intake and interaction of vitamin K with anti-coagulation medication. WF
Passwater: Let’s give our readers a break here and come back next month in Part 2 with a discussion of the research showing that nutritional levels of vitamin K2 can reverse calcium deposits in arteries, the effect of vitamin K2 on bone health. Also covered will be how vitamin K works in the body, what are adequate and optimal levels of vitamin K intake and interaction of vitamin K with anti-coagulation medication. WF
Dr. Richard Passwater is the author of more than 40 books and 500 articles on nutrition. He is the vice president of research and development for Solgar, Inc. Dr. Passwater has been WholeFoods Magazine’s science editor and author of this column since 1984. More information is available on his Web site, www.drpasswater.com
Published in WholeFoods Magazine, February 2009










