Last month, we began our conversation with Dr. Leon Schurgers about vitamin K2 with a discussion of the “calcium paradox,” in which so many people have harmful calcium deposits form in their arteries at the same time that the calcium content of their bones is decreasing. This calcium paradox is not a result of too little calcium in the diet, but of too little vitamin K2 that largely controls where the calcium goes. The objective is to keep calcium in our bones, not in our arteries. This is the role of vitamin K—putting calcium in its place!

Dr. Leon Schurgers is a senior scientist in biochemistry at the Maastricht University in The Netherlands. He is the vice president of VitaK Research at the Maastricht University, the world’s largest research institute dedicated to vitamin K.
Furthermore, as a senior scientist for the Division on Vitamin K Research, Dr. Schurgers is part of the Cardiovascular Research Institute (CARIM), the largest research institute of the University of Maastricht. Leading the scientific part on vitamin K-research and supervising technical engineers, post-docs and Ph.D. students is Dr. Schurgers’s major occupation. Dr. Schurgers is a member of the American Society of Bone and Mineral Research, the International society on Thrombosis and Haemostasis as well as the American Heart Association. He has published over 50 research papers in the international scientific press.
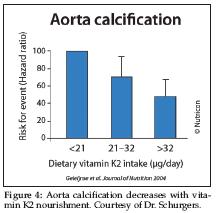
 In part 1 of this interview (published last month in WholeFoods Magazine), Dr. Schurgers was kind enough to share with us a photo that clearly demonstrates that vitamin K2-deficient aortas calcify whereas adequately vitamin K2-nourished aortas are calcification free. Let’s translate the photograph into numbers. Figure 4 is a graph showing the correlation of vitamin K2 level with decreased calcification of the aorta.
In part 1 of this interview (published last month in WholeFoods Magazine), Dr. Schurgers was kind enough to share with us a photo that clearly demonstrates that vitamin K2-deficient aortas calcify whereas adequately vitamin K2-nourished aortas are calcification free. Let’s translate the photograph into numbers. Figure 4 is a graph showing the correlation of vitamin K2 level with decreased calcification of the aorta.
More importantly, the risk of dying from cardiovascular disease decreases with increasing vitamin K2 levels. Figure 5 clearly shows this relationship.
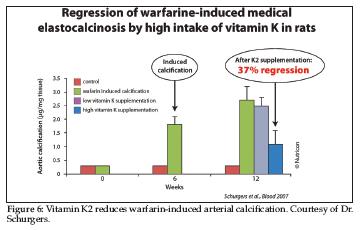
Passwater: In Part 1, you discussed your research showing that vitamin K2 prevented the calcification of arteries that occurs when warfarin is taken. We’ll discuss the warfarin–vitamin K interaction shortly, but in essence, warfarin induces calcification in arteries as warfarin blocks vitamin K’s ability to activate MGP. Would you elaborate on this study for us?
 Schurgers: We use warfarin to experimentally induce arterial calcification. In this study, we gave warfarin to control animals together with vitamin K1 to prevent bleeding. After stopping the warfarin plus vitamin K1 regimen, we continued with high vitamin K2 supplementation. Figure 6 shows the results graphically. Vitamin K2 reduces the arterial calcification caused by the warfarin. This is a good model to demonstrate how vitamin K2 reduces arterial calcification due to a vitamin K2 shortage.
Schurgers: We use warfarin to experimentally induce arterial calcification. In this study, we gave warfarin to control animals together with vitamin K1 to prevent bleeding. After stopping the warfarin plus vitamin K1 regimen, we continued with high vitamin K2 supplementation. Figure 6 shows the results graphically. Vitamin K2 reduces the arterial calcification caused by the warfarin. This is a good model to demonstrate how vitamin K2 reduces arterial calcification due to a vitamin K2 shortage.
Passwater: Can calcium accumulation reversal be achieved with nutritional levels of vitamin K2? Currently, there is no RDA for vitamin K as the Food and Nutrition Board of the Institute of Medicine is of the opinion (as of 2001) that there is only sufficient scientific evidence to establish an “Adequate Intake” (AI) of 120 mcg f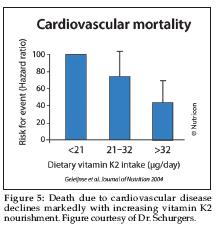 or men and 90 mcg for women. This should be adequate for the activation of the blood-coagulation factors, but I feel that more is needed for optimal bone and artery health. As a note to our readers, the Food and Nutrition Board is a scientific body and is not to be confused with the U.S. Food and Drug Administration’s “US RDA” established in 1973 as a reference for use in nutritional labeling and other regulations involving nutrition components. The US RDAs are set based on the Food & Nutrition Board’s recommendations, but in the case of vitamin K, the FDA appears woefully out of date.
or men and 90 mcg for women. This should be adequate for the activation of the blood-coagulation factors, but I feel that more is needed for optimal bone and artery health. As a note to our readers, the Food and Nutrition Board is a scientific body and is not to be confused with the U.S. Food and Drug Administration’s “US RDA” established in 1973 as a reference for use in nutritional labeling and other regulations involving nutrition components. The US RDAs are set based on the Food & Nutrition Board’s recommendations, but in the case of vitamin K, the FDA appears woefully out of date.
Schurgers: For the general healthy population, natural vitamin K2 will be effective in nutritional (physiological) dosages, which fits in the current official recommendations. As Figure 4 shows, the data from the Rotterdam Study nicely show that the regular consumption of 45 mcg vitamin K2 per day reduced the incidence of calcification by 50%.
Passwater: Do these nutritional levels present a problem to people on anticoagulation medication? Oral 4-hydroxycoumarin derivatives such as warfarin are widely prescribed anticoagulants for the treatment of thrombotic disorders. Warfarin is also commonly used as a rodent poison as large quantities can cause them to bleed to death. These drugs inhibit the body’s cycling of vitamin K to the active form that assists in the gamma-carboxylation of specific proteins such as procoagulants, osteocalcin and MGP. Earlier, you mentioned inducing arterial calcification by using warfarin.
 Schurgers: Today, we find daily intakes of 45 mcg of vitamin K2 do not interfere with anticoagulation medication. It is known that the high intake of vitamin K (either K1 or K2) overcomes the anticoagulant effect of coumarins. As long as coumarins such as warfarin are around, interference with vitamin K (whatever form) will be an issue. I am very confident that most people will switch in the near future from coumarin to specific oral anticoagulants such as dabigatran, which may not be available in the United States yet. Dabigatran has been marketed as Pradaxa since April 2008 in European countries and as Pradax in Canada. For now, we advise people on oral anti-coagulant medication to consult their medical doctors.
Schurgers: Today, we find daily intakes of 45 mcg of vitamin K2 do not interfere with anticoagulation medication. It is known that the high intake of vitamin K (either K1 or K2) overcomes the anticoagulant effect of coumarins. As long as coumarins such as warfarin are around, interference with vitamin K (whatever form) will be an issue. I am very confident that most people will switch in the near future from coumarin to specific oral anticoagulants such as dabigatran, which may not be available in the United States yet. Dabigatran has been marketed as Pradaxa since April 2008 in European countries and as Pradax in Canada. For now, we advise people on oral anti-coagulant medication to consult their medical doctors.
Passwater: Interesting! Around Thanksgiving time, a message went out to hospitals to make them in compliance with a national Joint Commission requirement regarding vitamin K-controlled diets for warfarin patients. Most patients on warfarin are warned not to consume “cranberry juice and dark greens such as spinach, broccoli and collard greens.” This advice will have detrimental effects on bones, arteries and heart valves. It is better to consume a constant intake of vitamin K and balance the ratio of warfarin –to–vitamin K with the International Normalized Ratio.
For normal healthy persons, there are no known adverse effects due to dosage as vitamin K has no activity other than gamma-carboxylation of certain proteins, and once they are 100% carboxylated, no other action occurs.
Schurgers: The U.S. Food and Nutrition Board of the Institute of Medicine has not set an Tolerable Upper Intake Level as no adverse effect has been reported for healthy individuals consuming vitamin K.
Passwater: What is the difference between vitamin K1 and vitamin K2?
Schurgers: As Figure 2 in Part 1 shows, vitamins K1 and K2 are structurally related compounds exhibiting the same function: activation of vitamin K-dependent proteins. They differ, however, in the side chain and thus in lipophylicity. Because of this difference, vitamins K1 and K2 have different bioactivities, efficacies and bioavailabilities. Our research has shown that due to this difference, vitamin K1 is poorly absorbed (only some 15%) because of its tight binding to the chloroplast membrane. Moreover, vitamin K1 is not redistributed by the liver, and thus its main effect is the activation of vitamin K-dependent clotting factors in the liver. On the other hand, vitamin K2—due to its lipophylic character—is not only used by the liver but also redistributed via blood in VLDL and LDL. Therefore, vitamin K2 is very accessible for extra-hepatic tissues such as bone and vessel walls.
Passwater: What are good natural food sources of vitamin K2?
 Schurgers: Vitamin K1 is found in green leafy vegetables, where it is tightly bound to the chloroplast membrane. Vitamin K2 is of bacterial origin. Therefore, we find it in fermented food products, where the bacteria are used as starters for fermentation culture. Typical fermented foods are cheese, curd cheese and sauerkraut. The best source of vitamin K2 is the traditional Japanese dish natto. Natto is a fermented soy bean that is very popular in Japan, but not appreciated outside Japan. Now, this special vitamin K2 is available as supplement without any smell and taste. Small amounts of both K1 and K2 can be found in various animal products as animals consume plant-form vitamin K1 and absorb vitamin K2 from their intestinal tracts.
Schurgers: Vitamin K1 is found in green leafy vegetables, where it is tightly bound to the chloroplast membrane. Vitamin K2 is of bacterial origin. Therefore, we find it in fermented food products, where the bacteria are used as starters for fermentation culture. Typical fermented foods are cheese, curd cheese and sauerkraut. The best source of vitamin K2 is the traditional Japanese dish natto. Natto is a fermented soy bean that is very popular in Japan, but not appreciated outside Japan. Now, this special vitamin K2 is available as supplement without any smell and taste. Small amounts of both K1 and K2 can be found in various animal products as animals consume plant-form vitamin K1 and absorb vitamin K2 from their intestinal tracts.
Passwater: Do we need to consume both K1 and K2 or would K2 be able to satisfy all of vitamin K needs?
 Schurgers: That is a good question! Since vitamin K2 is taken up by the liver and redistributed in the circulation via LDL, all tissues bearing an LDL receptor can make use of this vitamin. This includes bone, vasculature and liver. Moreover, due to its very long half-life in the circulation (> 3 days), it is available for all tissues 24 hours a day. So, if we take natural vitamin K2, no extra supplemental K1 is needed.
Schurgers: That is a good question! Since vitamin K2 is taken up by the liver and redistributed in the circulation via LDL, all tissues bearing an LDL receptor can make use of this vitamin. This includes bone, vasculature and liver. Moreover, due to its very long half-life in the circulation (> 3 days), it is available for all tissues 24 hours a day. So, if we take natural vitamin K2, no extra supplemental K1 is needed.
Passwater: You have mentioned matrix Gla protein (MGP) twice. MGP is a protein that carries calcium similar to a chelate that holds calcium “in its claws,” but it doesn’t do this unless the MGP is “activated” by vitamin K. This is a critical finding. What is this all about?
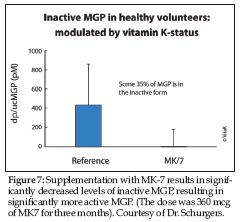
Schurgers: Vitamin K achieves a process on the proteins called “carboxylation.” Carboxylation gives the proteins claws so they can hold onto calcium. Once the protein grabs onto calcium, it can be moved. Gamma-carboxylation is catalyzed by the vitamin K-dependent gamma-carboxylase. If there is not enough vitamin K2 in the blood, then some of the MGP will remain inactive and won’t be able to do its job of putting calcium where it belongs. Figure 7 shows this relationship.
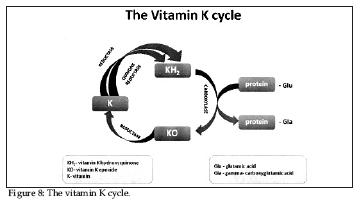
Passwater: In order to gamma-carboylate MGP, vitamin K itself must cycle between various forms as shown in Figure 8.
 Schurgers: The reduced form of vitamin K, vitamin K hydroquinone (vitamin KH2), is the actual cofactor for the gamma-carboxylases as it is converted to vitamin K epoxide. Proteins containing gamma-carboxyglutamate are called Gla proteins. The two vitamin K-dependent proteins found in bone are osteocalcin, also known as bone Gla (gamma-carboxyglutamate) protein or BGP, and the matrix Gla protein or MGP.
Schurgers: The reduced form of vitamin K, vitamin K hydroquinone (vitamin KH2), is the actual cofactor for the gamma-carboxylases as it is converted to vitamin K epoxide. Proteins containing gamma-carboxyglutamate are called Gla proteins. The two vitamin K-dependent proteins found in bone are osteocalcin, also known as bone Gla (gamma-carboxyglutamate) protein or BGP, and the matrix Gla protein or MGP.
Passwater: MGP and osteocalcin are both calcium-binding proteins that may participate in the organization of bone tissue. Several nutrients (including the major minerals calcium and phosphorus) are essential for bone health, but bone tissue is organic, not just mineral. Bone consists of a matrix of proteins that holds the minerals together. Vitamin C is needed for collagen cross-linking. Copper, zinc, manganese and boron are needed as co-factors for the enzymes that act in the synthesis or post-translational modification of constituents of bone matrix. Silicon is needed for collagen production and to act as a cross-linking agent to stabilize the glycosaminoglycan network. Vitamin D is needed to produce osteocalcin. Even if you have more than enough calcium, vitamin D and osteocalcin in your blood, bone formation will be greatly impaired without adequate vitamin K to activate the osteocalcin so that it takes the calcium from the blood and puts the calcium into the bone tissues.
What human evidence is there that vitamin K2 helps maintain bone mineral density?
Schurgers: Several clinical intervention trials have been conducted to show the beneficial effect of vitamin K. Whereas vitamin K1 was shown to reduce bone loss by 35%, vitamin K2 could completely prevent the loss of bone strength in postmenopausal women. The effect of vitamin K is via the activation of the vitamin K-dependent bone protein called osteocalcin. As Figure 8 shows, we and others have shown that in the normal population, some 30% of osteocalcin is in the inactive form. Therefore, extra vitamin K is needed to reduce this fraction.
 Passwater: Since the bone-forming and mineralization cells called osteoblasts produce osteocalcin and osteocalcin is inactive until activated by vitamin K, is there evidence that vitamin K2 can overcome osteoporosis?
Passwater: Since the bone-forming and mineralization cells called osteoblasts produce osteocalcin and osteocalcin is inactive until activated by vitamin K, is there evidence that vitamin K2 can overcome osteoporosis?
Schurgers: Osteoporosis is a disease in which the bone mineral density is extremely low. Our studies always focused on postmenopausal women, in which bone loss is accelerated. We wanted to demonstrate that extra vitamin K could reduce this bone loss and prevent women from becoming osteoporotic. Once women are osteoporotic, we would advise them to visit their medical doctors.
Passwater: Who should consider taking vitamin K2 supplements?
Schurgers: Recent scientific data show even a well-balanced diet might not provide sufficient vitamin K to fulfill the body’s needs. Measuring vitamin K-dependent proteins in many apparently healthy subjects showed that people that do not consume vitamin K-supplements have some 30% inactive vitamin K-dependent proteins. As these inactive proteins are correlated with bone and vascular disease, everybody should consider taking some extra vitamin K2. In this way, we can remove this risk factor.
Passwater: What type of vitamin K supplement is best?
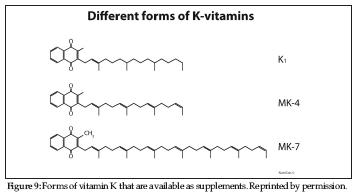
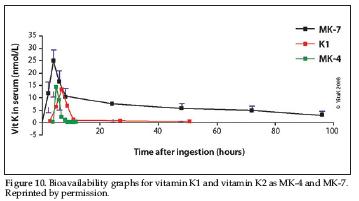
Schurgers: Currently, there are three types of vitamin K available as supplements including synthetic vitamin K1, menaquinone-4 (MK-4), a vitmain K2 that is not extracted from a natural food source, and natural vitamin K2 as menaquinone-7 (MK-7) as shown in Figure 9. Due to the deficiency of K vitamins in most people as a result of the Western diet, I recommend supplementation for optimal bone and cardiovascular health. If you have a choice, vitamin K2 is preferable to K1, as K2 intake has been linked to both bone and cardiovascularhealth. And, as Figure 10 shows, the most desirable form of K2 is natural vitamin K2 as MK-7, as this is the most bioavailable, bioactive and longest lasting form of vitamin K available. Our laboratory has tested one MK-7 product (MenaQ7) for safety and efficacy in humans, and thus I can recommend it.
 Passwater: Where does your research take you next?
Passwater: Where does your research take you next?
Schurgers: I am currently preparing and planning three big clinical trials with medical doctors: one trial in aortic stenosis patients (cardiology department), one in dialysis patients (a multicenter trial including some 500 patients) and one trial in cardiac patients with calcifications and hypertension. All trials will be conducted with 360 mcg of MK-7.
Passwater: This will be very important research. I know of a lot of women who would appreciate seeing a study of vitamin K2 versus breast soft-tissue califications. Biochemistry logic suggests that vitamin K2 could reduce breast calcifications and thus, reduce the need for many biopsies.
Thank you, Dr. Schurgers, for your research and for chatting with us about the importance of vitamin K2 in bone and artery health. I know our readers are looking forward to chatting with you again as more of your research is finished, and, perhaps we can also include a discussion about the workings of the vitamin K cycle. Readers can find more information about vitamin K2 at http://vitamink2.org. WF
Dr. Richard Passwater is the author of more than 40 books and 500 articles on nutrition. He is the vice president of research and development for Solgar, Inc. Dr. Passwater has been WholeFoods Magazine’s science editor and author of this column since 1984. More information is available on his Web site, www.drpasswater.com
Published in WholeFoods Magazine, March 2009










