The running joke is that women are natural-born shoppers, obsessed with malls and fearless in the face of a crowded sale or 10-person-deep checkout line. According to a new Facts, Figures & the Future e-newsletter, there’s some truth to this.
While men may be shopping more these days, women are still making the majority of the purchasing decisions for their families. In a study of women with children under the age of 18, females made 72% of visits to dollar stores and mass merchants in 2012, 69% of trips to supercenters, 68% to drug stores, 63% to supermarkets, 61% to wholesale clubs and 43% to convenience/gasoline outlets (1). And, they tend to outspend male shoppers by about 39%.
Given this powerful and engaged group of shoppers, it’s essential that you offer a host of products to meet women’s most important health needs in your store.
Making PMS a Thing of the Past
If you were to look at the ingredients in a top-selling anti-PMS drug, you’d find acetaminophen (to cover up pain), as much caffeine as a cup of coffee (to act as a diuretic) and possibly an antihistamine (to put you in a fog and “reduce tension”).
It shouldn’t surprise you that many women aren’t  interested in taking these overpriced painkillers, and would love to hear about natural approaches to deal with premenstrual syndrome. As it turns out, there are many nutritional links to PMS, particularly with deficiencies. States Michael Mooney, director of research and education at SuperNutrition, Oakland, CA, “Published studies show reductions in PMS discomfort if you take the right potencies of several easy-to-find dietary supplements.”
interested in taking these overpriced painkillers, and would love to hear about natural approaches to deal with premenstrual syndrome. As it turns out, there are many nutritional links to PMS, particularly with deficiencies. States Michael Mooney, director of research and education at SuperNutrition, Oakland, CA, “Published studies show reductions in PMS discomfort if you take the right potencies of several easy-to-find dietary supplements.”
Mooney zeroes in on five vitamins/minerals that may help women avoid PMS discomfort:
• In a study of 630 women, daily vitamin B6 intake (160–200 mg) reduced PMS discomfort in about 79% of the subjects (2). Mooney says even smaller amounts (100–150 mg) were helpful for about 66% of the women.
• According to data from the Nurses’ Health Study II, women who took at least 706 IU of vitamin D daily had significantly less discomfort than those who consumed less (112 IU) (3).
• Calcium supplements (1,000 mg daily) may help, and Mooney cites a placebo-controlled study in which 58% of women benefited from it (4). “Both water retention and pain scores were significantly reduced by calcium carbonate supplementation,” he states.
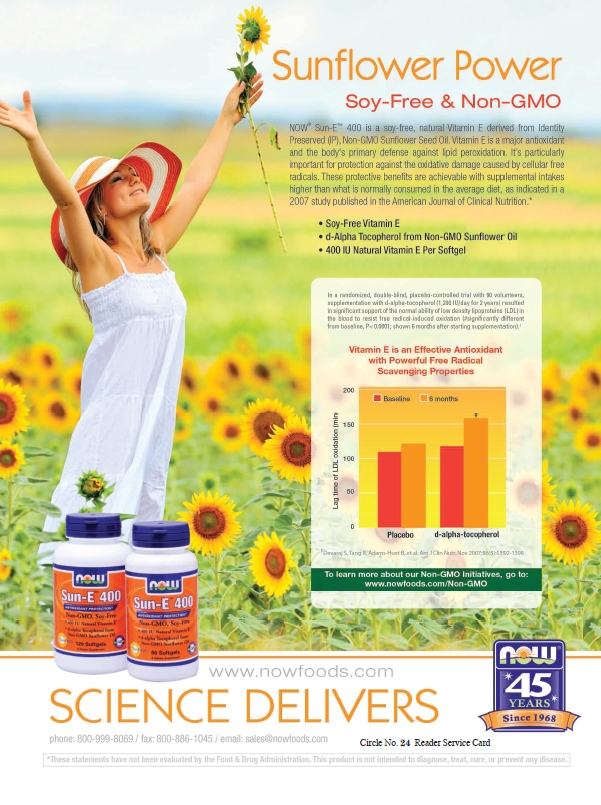
• Researchers found vitamin E (400 IU/day) reduced PMS symptoms by 27–42% (5).
• Last, Mooney says magnesium (360 mg/day) helped reduce headaches in one study (6) and fluid retention (200 mg/day) in another (7).
But, vitamins and minerals aren’t the only options; herbs like vitex are said to reduce PMS discomfort. In one study, states Mooney, women taking 20 mg/day of the herb for three months had a 28% reduction in irritability, mood disturbances, anger, headache and breast fullness compared to the placebo group (8).
How fast should women expect to experience relief from PMS symptoms? According to Mooney, it could take a few months. He states, “Studies are clear that the nutritional supplements that help reduce PMS symptoms work better over time, with the maximum effect happening after taking them consistently for three cycles.”
Getting Back in the Mood
Many women find that once the perimenopause years hit (when cycles become irregular), their sexual vitality isn’t what it used to be. In fact, surveys referenced by Dallas Clouatre, Ph.D., consultant for R&D at Jarrow Formulas, Inc., Los Angeles, CA, indicate about one-third of women going through perimenopause lose their libido. The number jumps to half for women who have completed menopause.
 Getting in the mood may be tough during perimenopause, menopause and thereafter for several reasons. These include trouble sleeping, reduced energy levels and declining health as a natural consequence of aging, says Clouatre.
Getting in the mood may be tough during perimenopause, menopause and thereafter for several reasons. These include trouble sleeping, reduced energy levels and declining health as a natural consequence of aging, says Clouatre.
Another potential cause has to do with hormones. “The changes of hormones, both month-to-month and as they age over the decades, affect women in profound ways,” says Neil E. Levin, CCN, DANLA, nutrition education manager at NOW Foods, Bloomingdale, IL. This includes everything from desire to arousal times to vaginal lubrication.
Hormones that regulate libido include estrogen, progesterone and testosterone. “They exercise different, yet sometimes overlapping roles in determining sex drive,” states Clouatre. For instance, testosterone elevates mood, but its production lessens with age, which can affect libido.
Marita Schauch, N.D., women’s health educator for Natural Factors, Monroe, WA, says testosterone levels are directly tied to sex drive in both genders. “Testosterone is also responsible for sexual desire, arousal and sexual sensation,” Schauch explains. “Declining testosterone levels have been associated with a decrease in libido.”
Meanwhile, Clouatre explains that estrogen—another mood elevator—“keeps vaginal and urethral tissues more ‘full’ with adequate moisture for normal intercourse.”
But during perimenopause, levels drop. Without this moisture, intercourse can be unpleasant, so much so that it lessens a woman’s interest in sexual activity. States Schauch, “A loss of estrogen can manifest as vaginal dryness, loss of elasticity, bleeding after intercourse and painful sex.”
Dealing with dryness, states Tracey Saenz, vice president and general manager of consumer products at Evofem, San Diego, CA, is all about taking preventative measures. She states, “Soy and flaxseeds are good sources of phytoestrogens, which you can include in your diet to help balance your hormones.”
Feminine hygiene products may also affect vaginal dryness. Saenz believes using absorptive synthetic tampons can exacerbate dryness, “especially with frequent changing or on light flow days.”
A suitable alternative could be menstrual cups, which catch menstrual blood as opposed to soaking it up. Says Saenz, “When inserted correctly, it can’t be felt, and it doesn’t absorb the body’s natural moisture. It can be worn up to 12 hours during heavy or light flow.”
which catch menstrual blood as opposed to soaking it up. Says Saenz, “When inserted correctly, it can’t be felt, and it doesn’t absorb the body’s natural moisture. It can be worn up to 12 hours during heavy or light flow.”
Sophie Zivku, M.A., communications and education manager at Diva International Inc., Kitchener, ON, Canada, feels the same way about the benefits of a menstrual cup: “It will not dry out or disrupt the natural environment or pH of the vagina.”
Zivku says the material of her company’s product makes a difference, too. “Unlike the abrasive material of synthetic fibers commonly found in tampons, because of its silicone composition, The DivaCup is very comfortable and collects, not absorbs, menstrual flow, helping to maintain the natural environment of the vaginal canal.”
But, it would be a mistake to classify all tampons and pads as unsuitable for women experiencing dryness. Part of the issue is about the materials used in such products. For instance, drug-store varieties have been bleached and contain harmful chemicals. According to material supplied by Natracare (9), “Most conventional sanitary pads and some claiming to be ‘natural’ are made from over 90% plastic manufactured from crude oil, including polyacrylate super absorbents, polyethylene and polypropylene.” Not only is this a problem for the environment (as Natracare says that the production of plastic and polypropylene releases toxic chemicals and the plastic itself never biodegrades), but it also spells trouble for a woman’s body.
Conversely, Rebecca Alvandi, vice president of Maxim Hygiene Products, Roslyn Heights, NY, says women often find relief from conditions like vaginal dryness with her company’s organic and natural cotton tampons and pads.
“There is a growing population of women who are becoming more and more sensitive to the irritating materials found in conventional products,” states Alvandi. “Symptoms include rashes, odor and infections caused by plastic-laden sanitary pads that create the perfect microclimate for the proliferation of bacteria; all of which detours any possibility or desire for sexual interaction.”
Part of the reason has to do with the fibers found in the center/absorbent cores of conventional pads, Alvandi says. These pads have smaller dust-like particles such as wood pulp, she explains, which are not breathable and are irritating.
 She believes making feminine hygiene products with organic and natural cotton helps create a naturally hypoallergenic and breathable end product that “not only helps prevent the risk of irritation, but also helps soothe it.” Natural cotton products have long linear fibers that contribute to their breathability. “Breathability is especially important for women with skin sensitivities because it means air can flow freely, which feels soothing and prevents bacteria build up,” Alvandi states.
She believes making feminine hygiene products with organic and natural cotton helps create a naturally hypoallergenic and breathable end product that “not only helps prevent the risk of irritation, but also helps soothe it.” Natural cotton products have long linear fibers that contribute to their breathability. “Breathability is especially important for women with skin sensitivities because it means air can flow freely, which feels soothing and prevents bacteria build up,” Alvandi states.
Natracare warns retailers to be sure the cotton used in feminine hygiene products is free of chlorine in every aspect from the absorbent core to the packaging. This company’s pads and liners are “made from renewable, sustainable and biodegradable materials” such as plant-derived cellulose and organic cotton sourced ecologically. The choice is important because bleaching with chlorine produces dioxins, which are carcinogenic and harm the environment.
Other ways to deal with menopause symptoms include hormone replacement therapy (HRT) for increasing energy and libido. “But, this pharmaceutical approach has equally well-known adverse effects,” states Paul Clayton, chief scientific advisor at Gencor Nutrients, Anaheim, CA.
Luckily, several supplements support women going through perimenopause by helping maintain hormonal balance as long as possible.
For instance, Clayton highlights the benefits of sterols derived from a specific strain of fenugreek: “These valuable molecules displace a small percentage of estradiol [i.e., an important form of estrogen] from binding proteins in the blood, known as SHBG and serum albumen; and this approach, in pre-menopausal women, pushes free estradiol levels toward the top of the normal range.”
In the end, this means that high serum levels of estradiol aren’t reached, as in the case of dangerous pharmaceuticals. So, with the natural fenugreek method, women achieve a gentle, safe increase in sexual vitality.
Another option, according to Cheryl Myers, chief of education and scientific affairs at EuroPharma, Inc., Green Bay, WI, is maca. This may surprise you as an option in the women’s category. “While many people consider maca a ‘men only’ supplement, nothing could be further from the truth,” she states.
Myers explains that maca helps support healthy  energy and stamina levels, which is something many women need to regain some sexual vitality. “I think it’s safe to say that most people feel much more ‘in the mood’ when they aren’t exhausted by the demands of the day,” states Myers.
energy and stamina levels, which is something many women need to regain some sexual vitality. “I think it’s safe to say that most people feel much more ‘in the mood’ when they aren’t exhausted by the demands of the day,” states Myers.
One study on maca root (10) involved giving 20 individuals either a low dose (1.5 g/day) or a high dose (3.0 g/day). The group (mostly women) had been using selective serotonin reuptake inhibitors (SSRI) antidepressant drugs, which caused a decrease in sexual desire. In the end, the higher dose significantly improved libido.
Myers also feels that omegas from sea buckthorn are valuable for menopause support because they are very lubricating. “This complete sea buckthorn extract promotes healthy mucosal membranes in the vagina,” she states. “In fact, this extract has been shown to reduce the burning, itching and dryness of Sjögren’s syndrome.” Myers feels so strongly about the benefits of omegas that she believes it should be taken proactively to avoid vaginal dryness.
Given the relationship between hormonal changes and vaginal dryness, Schauch believes rhodiola, suma, eleuthero, schisandra and ashwagandha are all good for supporting the fluctuations in estrogen and testosterone as well as supporting healthy adrenal function. She explains that about half of a woman’s testosterone comes from her ovaries and adrenal glands. “Therefore, supporting healthy adrenal function is also important to optimize sexual desire as well as other menopausal symptoms,” says Schauch.
Some women may also prefer topical products like a high-quality vaginal lubricant. Says Saenz, “Try a lubricant without the parabens and other xenoestrogens that act as hormone disruptors.”
Amy Spreadborough, marketing manager for Emerita/Nutraceutical Corporation, Portland, OR, says her company offers a lubricant with aloe and vitamin E for tissue support and also a moisturizing gel that offers aloe, ginseng, calendula, chamomile and vitamin E for maintaining balance and comfort.
For those looking for a libido boost, the company has a warming lubricant, “which can help get things going in a natural way,” says Spreadborough, and a topical arousal cream that incorporates rosemary and niacin for a mild, tingling sensation.
Another option is a natural progesterone cream, which is said to help with hormonal balance since progesterone is a precursor to several other hormones.
Too Hot to Handle
Have you had female clientele complain of menopause-related hot flashes? There are several ways your store can help.
 “Hot flashes and night sweats are reported by about 85% of menopausal women and are related to the decline in ovarian function,” states Schauch. “The clearest explanation for hot flashes is that they appear to be the body’s response to a sudden downward resetting of the body’s thermostat, which is located in the hypothalamus.” She adds that low estrogen and progesterone levels may also be linked with hot flashes.
“Hot flashes and night sweats are reported by about 85% of menopausal women and are related to the decline in ovarian function,” states Schauch. “The clearest explanation for hot flashes is that they appear to be the body’s response to a sudden downward resetting of the body’s thermostat, which is located in the hypothalamus.” She adds that low estrogen and progesterone levels may also be linked with hot flashes.
But, low estrogen levels alone is not the whole story, according to Eileen Sheets, managing director of Bioforce USA, Ghent, NY: “It appears the withdrawal of estrogen during menopause may be the trigger.” However, she speaks of new research indicating a group of brain cells found in the hypothalamus (called KNDy neurons) may be the “control switch” of hot flashes.
Another aspect of hot flashes could be related to changes in circulation, states Alexis Harwood, senior brand manager, Reserveage Organics, Gainesville, FL.
And, Rafael Avila, manager of research and development at Natural Organics, Inc., Melville, NY, adds that the flushing some women experience happens when the blood vessels near the skin’s surface dilate to cool down the body. He states, “This produces the red, flushed look to the face. A woman may also perspire to cool down the body. In addition, some women experience a rapid heart rate or chills.”
• He believes that natural supplements can help, such as the vitamin B complex and vitamin E.
• Black cohosh is often recommended to women experiencing  hot flashes. According to Mooney, one study of 149 perimenopausal and postmenopausal women found the herb was as effective at a low dose of 39 mg per day in 70% of the group as it was at 127 mg/day (11). Susan Hazels Mitmesser, Ph.D., director of nutrition research at Solgar, Leonia, NJ, also weighs in: “Black cohosh contains triterpene glycosides, phytochemicals that contribute to the plant’s ability to positively influence the natural changes that occur before, during and after menopausal years.”
hot flashes. According to Mooney, one study of 149 perimenopausal and postmenopausal women found the herb was as effective at a low dose of 39 mg per day in 70% of the group as it was at 127 mg/day (11). Susan Hazels Mitmesser, Ph.D., director of nutrition research at Solgar, Leonia, NJ, also weighs in: “Black cohosh contains triterpene glycosides, phytochemicals that contribute to the plant’s ability to positively influence the natural changes that occur before, during and after menopausal years.”
• Some other suggestions come from Schauch, who recommends sage, vitex, dong quai, red clover and phytoestrogens, which she believes support the fluctuating estrogen and progesterone levels that may trigger hot flashes. “Some women going through menopause try to get relief from their symptoms from natural alternatives or supplements that include phytoestrogens, or natural estrogens,” states Harwood, noting that an allergen-free form of genistein may provide relief against menopausal symptoms. Sheets agrees about sage, adding that an eight-week study done on organic sage offered by her company (A Vogel Menopause Tablet) found a 46% decrease in mild hot flashes, a 62% decrease in moderate hot flashes, a 79% decrease in severe hot flashes and a 100% decrease in very severe hot flashes.
• Myers believes hops cone extract shouldn’t be overlooked for hot flashes, citing a study on a product marketed by her company: “The use of the unique hops extract in MenoComplete was associated with four times fewer hot flashes and double the reduction in overall menopause symptoms (versus placebo).”
• Michael Jeffers, CEO of Helios Corp., Santa Fe, NM, says a branded combination of three herbs (Phlomis umbrosa, Cynanchum wilfordii and Angelica gigas Nakai, as EstroG-100) provides an alternative to isoflavones and black cohosh. He says it works quickly on symptoms like vaginal dryness and hot flashes. “EstroG-100 was proven to work on one or more symptoms in seven to 10 days whereas post WHI compounds in the public domain such as black cohosh and genistein, and siberian rhubarb worked in six weeks minimum,” states Jeffers.
 • Last, a branded French maritime pine bark extract (Pycnogenol, distributed by Horphag USA) may also reduce some menopause symptoms. The study (conducted at Keiju Medical Center in Japan) involved 170 perimenopausal women who took either a placebo or 30 mg of the extract twice daily for 12 weeks. Two significant findings were published. First, questionnaires suggested that the extract improved the comfort of women with perimenopausal symptoms. Second, the extract didn’t cause any hormonal effects. Stated Horphag USA in a press statement, “The evidence for non-hormonal effects of Pycnogenol may be welcomed by women who wish to soothe menopausal symptoms without using supplements containing soy, kudzu, red clover and other herbals to exert hormonal activity.”
• Last, a branded French maritime pine bark extract (Pycnogenol, distributed by Horphag USA) may also reduce some menopause symptoms. The study (conducted at Keiju Medical Center in Japan) involved 170 perimenopausal women who took either a placebo or 30 mg of the extract twice daily for 12 weeks. Two significant findings were published. First, questionnaires suggested that the extract improved the comfort of women with perimenopausal symptoms. Second, the extract didn’t cause any hormonal effects. Stated Horphag USA in a press statement, “The evidence for non-hormonal effects of Pycnogenol may be welcomed by women who wish to soothe menopausal symptoms without using supplements containing soy, kudzu, red clover and other herbals to exert hormonal activity.”
Also relevant for women with hot flashes are natural feminine hygiene products. Alvandi says women going through menopause may experience uncomfortable wetness. She states, “The need for 100% cotton-based products is strong in women who experience hot flashes and night sweats because the heat damp environment created by such symptoms encourages the growth of bacteria when combined with plastic synthetic materials; cotton is a more breathable fiber that allows air to flow through and soothe irritation and the uncomfortable wet feeling accompanying such symptoms.”
Bone Support for Women
While night sweats and loss of sexual vitality aren’t fun, they may be considered “inconveniences” of menopause compared with the potentially life-altering situations that bone loss can cause.
According to one study, bone loss accelerates in late perimenopause and continues to drop off at the same rate in the first few postmenopausal years (12). In total, women lose about half of their trabecular bone and 30% of their cortical bone throughout their lifetime—and about half of all this loss happens after menses stops (13).
“Osteoporosis presents a significant health problem to the United States,” states Hartley Pond, vice president of technical sales at VDF/FutureCeuticals, Momence, IL. “As a result, there is an ongoing, intense review of clinical data regarding osteoporosis, fractures and the role of diet and supplementation in prevention of bone loss.”
Calcium debate. Limiting this loss is a process that should start early, and one into which all your female clientele should enter. Of course, calcium, magnesium and vitamin D come to mind as important parts of this regimen. “Clearly, science has solidly established their efficacy in promoting bone mineralization (i.e., bone mass), and there is no question about the value of supplementing with these nutrients,” states Gene Bruno, M.S., MHS, director of category management at Twinlab Corporation, New York, NY.
But this doesn’t mean there isn’t more to learn; for instance, vitamin K (especially  the K2 form menaquinone-7) is essential for calcium metabolism. This is important because when calcium isn’t properly metabolized by the body, it could be harmful to cardiovascular health. According to Vladimir Badmaev, M.D., Ph.D., head of R&D at Nattopharma ASA, Oslo, Norway, a 2013 report from JAMA discusses the outcome of the National Institutes of Health (NIH)–AARP Diet and Health Study, which involved 219,059 men and 169,170 women followed for 12 years. “The outcome of the study revealed that intake of 1,000 mg per day of supplemental calcium from multivitamins or individual calcium supplements was associated with significant increase in heart disease death, primarily in men,” he states.
the K2 form menaquinone-7) is essential for calcium metabolism. This is important because when calcium isn’t properly metabolized by the body, it could be harmful to cardiovascular health. According to Vladimir Badmaev, M.D., Ph.D., head of R&D at Nattopharma ASA, Oslo, Norway, a 2013 report from JAMA discusses the outcome of the National Institutes of Health (NIH)–AARP Diet and Health Study, which involved 219,059 men and 169,170 women followed for 12 years. “The outcome of the study revealed that intake of 1,000 mg per day of supplemental calcium from multivitamins or individual calcium supplements was associated with significant increase in heart disease death, primarily in men,” he states.
Women are at risk, too, he believes, when they take calcium supplements without proper metabolizers like vitamins K2 and D. “These important epidemiological findings suggest that guidelines for calcium supplements may have to be revised, and calcium and vitamin D supplements may need to be complemented with vitamin K2 intake due to its known role as a calcium chaperone,” states Badmaev, adding that vitamin K helps protect against age-related cardiovascular deterioration and leads to improved bone and metabolic health.
Another possible factor in calcium metabolism is that D3 (cholecalciferol) is more active and potent than vitamin D2 (ergocalciferol) (14) and the jury is still out about which form of calcium is the best. According to Bruno, part of the reason for the debate may be that some research indicates that various forms of calcium (e.g., calcium citrate, calcium carbonate, hydroxyapatite, calcium gluconolactate and calcium pidolate) are absorbed at similar rates (15). Meanwhile, other studies suggest some forms (like calcium citrate) are better absorbed over others (such as calcium gluconolactate and carbonate) (16–18), states Bruno. Still other studies have found that calcium carbonate is fairly well absorbed when taken with a meal (19).
Sheets believes that intake of crude calcium doesn’t address calcium deficiency as well as other options, and an organically bound calcium from plant sources is needed. Her company uses stinging nettle, which is rich in calcium and silica. “The leaves contain up to 20% minerals in a very bioavailable form,” she states.
In the end, Bruno states, “The fact is that all of the research shows that these forms of calcium are absorbed, and have value for bone health.”
 Bruno says a differentiating point is that some calcium supplements may breakdown differently in the body than others. He suggests making sure that the manufacturer follows cGMPs and considering the delivery form. “There may also be an advantage in supplementing with calcium capsules versus tablets since capsules tend to dissolve more easily,” Bruno believes. “Another approach is to use chewable calcium wafers, thereby entirely eliminating the potential for poor tablet breakdown.”
Bruno says a differentiating point is that some calcium supplements may breakdown differently in the body than others. He suggests making sure that the manufacturer follows cGMPs and considering the delivery form. “There may also be an advantage in supplementing with calcium capsules versus tablets since capsules tend to dissolve more easily,” Bruno believes. “Another approach is to use chewable calcium wafers, thereby entirely eliminating the potential for poor tablet breakdown.”
Another calcium issue under scrutiny is whether high-dose calcium supplements are worth it, and this could be related to absorption issues. “A recent paper in the British Medical Journal linked high-dose supplementation of calcium with a significant increase in risk of heart disease in women,” states Pond. “A study done at Harvard and published in Journal of Nutrition pointed to the fact that countries with the highest rates of calcium intake also had some of the highest rates of large bone fractures in people with osteoporosis. The United States was at the top of both lists.”
Jeffers says there’s another point for debate: the indefinite claims made on labels. “Most label claims state ‘improves bone density,’ with consumption of a variety of calcium derivates or combinations plus D2 or magnesium, but we have seen nothing that can define what improvement is in these claims other than a definition about RDA levels for calcium intake and benefits of the D2 and magnesium in completely unrelated studies.” He believes there aren’t enough independent, unbiased clinical studies about whether calcium, calcium derivatives or calcium combinations build bone mass.
Jeffers feels an exception is an oyster shell-derived calcium carbonate from his company (NC-518), which is supported by human clinical studies to increase bone density by 2.2% over four months.
The hormone connection. Avila also believes taking calcium (along with important minerals like zinc and magnesium) “is a fantastic way to build bone mass.”
His company offers a formula with these  nutrients, but, interestingly, it’s not a bone-health product per se. “It’s designed to promote hormone health,” says Avila. “Given that bone health is directly associated with hormone health, particularly in women, one would expect that any supplement that improves hormone health must also improve bone health.”
nutrients, but, interestingly, it’s not a bone-health product per se. “It’s designed to promote hormone health,” says Avila. “Given that bone health is directly associated with hormone health, particularly in women, one would expect that any supplement that improves hormone health must also improve bone health.”
He believes some ingredients in the formula were chosen for their hormone-support properties, and they have since been found to promote bone health. “For example, a recent study showed that maca supplementation helps avoid bone loss due to estrogen depletion. Other studies suggest that dong quai, damiana and amino acids within the E Fem formula may also promote bone health,” Avila states.
Levin also speaks of the connection between hormones and bone health. “If dietary calcium is too low, the parathyroid hormone increases and actually dissolves bone to obtain more circulating calcium for other uses.”
W.H. Leong, vice president of Carotech Inc., Edison, NJ, adds some more information about the hormone–bone health connection. Estrogen regulates osteoclast (i.e., cells that break down bone) number and activity. “A decrease in estrogen level (for example, in the postmenopausal state) releases cytokines and thus increases osteoclasts’ life-span, subsequently leading to increased bone resorption, resulting in osteoporosis,” he states.
Benefiting osteoblasts. The bones are constantly remodeling and osteoblasts are responsible for bone formation. Thus, nutrients that support these critical cells are key for maintaining healthy bone mass.
Herb Joiner-Bey, N.D., scientific advisor to Barlean’s, Ferndale, WA, believes ALA from flax oil is key for this purpose. “Amazingly, every time lab animals have been given flaxseed oil as the major fat source, bone mineral density increases,” says Joiner-Bey.
He says ALA has a selective effect on osteoblasts and osteoclasts (which tear down bone tissue). States Joiner-Bey, “Miraculously, the flax oil omega-3 ALA inhibits the activity of osteoclasts and enhances the activity of osteoblasts.“
 Bruno believes soy-derived ipriflavone also supports osteoblasts’ function and inhibits bone resorption, mainly by inhibiting recruitment of osteoclasts; typically, results can be seen when 600 mg/day are used (20–22).
Bruno believes soy-derived ipriflavone also supports osteoblasts’ function and inhibits bone resorption, mainly by inhibiting recruitment of osteoclasts; typically, results can be seen when 600 mg/day are used (20–22).
He adds, “Likewise, soy isoflavones provide weak estrogenic effects on bone, resulting in significant support for bone density—with 80–120 mg typically used” (23–25).
Hazels Mitmesser adds another benefit of soy isoflavones for women’s health: “They contribute to bone health by helping to support calcium metabolism.”
Another bone-building nutrient is vitamin E tocotrienols. According to Leong, this form of vitamin E has been shown in osteoporosis studies to elicit more benefits for bone resorption than alpha-tocopherol vitamin E. The mechanism of action, he states, is by inhibiting osteoclast formation and activity.
Leong adds, “In a recent publication, researchers reported that in a postmenopausal osteoporosis rat model (overiectomized rats), supplementation of 60 mg/kg mixed tocotrienols for two months showed better overall bone parameters compared to estrogen-replacement therapy” (26).
Bone health and inflammation. Pond suggests another interesting way to handle bone health, and that’s with anti-inflammation support. “Formulators are looking beyond calcium supplementation and toward combinations with natural ingredients that can reduce inflammatory bio-markers that are closely associated with osteoporosis and bone loss,” Pond believes.
|
Select Women’s Health Offerings
Alvita: Raspberry and Red Clover teas. American Health: More Than A Multiple For Women, Ester-C 1,000 mg with D3 5,000 IU, Royal Brittany Evening Primrose Oil. Barlean’s: Barlean’s Essential Woman, Barlean’s Omega Swirl Essential Woman (Chocolate mint flavor), Barlean’s Forti-Flax (milled flaxseed), Brevail (flax lignan concentrate). Bioforce USA: Calcium Absorption Formula, Sage Menopause Tablets, Valerian Complex , Stress Management Drops. Carotech Inc.: Tocomin SupraBio (ingredient for manufacturers). Diva International: The DivaCup and DivaWash. Emerita/Nutraceutical Corporation: Natural Lubricant 2-oz., OH Warming Lubricant 2-oz., Response Topical Arousal Cream 1-oz., Libido Formula 30-ct., Personal Moisturizer 2-oz and 4-oz., Feminine Cleansing & Moisturizing Wash 4-oz., Feminine Cleansing and Moisturizing Cloths 6-ct or 15-ct., Menstrual Comfort Cream 2-oz., line of all-cotton feminine hygiene products. EuroPharma, Inc.: Andes Organic Maca, MenoComplete, Omega7, Evofem: Instead Softcup, in disposable and reusable options. Gencor: Libifem and Genopause ingredients. Helios Corp.: EstroG-100, NC-518 and TransportC-PLUS ingredients. Horphag: Pycnogenol. Jarrow Formulas: BONE-UP, BroccoMax, DIM + CDG, Iso-Rich Soy. Maxim Hygiene Products: Line of organic and natural chlorine-free cotton products, including tampons, sanitary napkins, panty liners and cosmetic accessories. Natracare: Chlorine-free line of feminine hygiene products made with organic cotton. Nattopharma ASA: MenaQ7 brand of vitamin K2. Natural Factors: WomenSense EstroSense, WomenSense AdrenaSense, WomenSense MenoSense, WomenSense ThyroSense, WomenSense RxOmega-3, BioSil. Natural Organics, Inc.: AgeLOSS Women’s Multi and Nature’s Plus E-Fem. NOW Foods: NOW Herbal Pause, NOW Menopause Support, NOW Natural Progesterone Liposomal Skin Creams, Chaste Berry-Vitex Extract 300 mg capsules, Dong Quai 520 mg capsules, Evening Primrose Oil softgel capsules, Ipriflavone 300 mg capsules, Soy Isoflavones capsules, Female Balance capsules with Wild Yam, Vitex, Dong Quai, and GLA. Solgar: SFP Black Cohosh Root Extract Vegetable Capsules, Non-GMO Super Concentrated Isoflavones Tablets, PM PhytoGen Complex Tablets (Pueraria mirifica), Prenatal Nutrients Tablets, Female Multiple Tablets, CRAN FLORA with Probiotics Plus Ester-C Vegetable Capsules, SFP Herbal Female Complex Vegetable Capsules. Reserveage Organics: Menopause Advantage. SuperNutrition: SimplyOne Women, SimplyOne 50+ Women, Women’s Blend, PreNatal Blend, Menopause Multiple and Calcium Blend. Twinlab Corporation: Twinlab Bone Support with Ostivone, Twinlab Calcium Citrate Caps, Twinlab Calcium Citrate Chewable Wafers. VDF/FutureCeuticals: Soylac Organic Fermented Soy Powder, Aglycone Soy Isoflavones 40%, FruiteX-B (calcium fructoborate), VitaCran Cranberry. |
|
He cites a recent article from a journal called Medical Hypotheses in which the author writes that inflammation plays a role in the advancement of osteoporosis (27). “In particular, high levels of C-reactive protein (CRP) are associated with lower bone mineral density,” states Pond.
He says his company has been investigating whether a plant-based calcium fructoborate (FruiteX-B) can help. Pond says three published studies suggest the ingredient can slash CRP levels by 40–60% and reduce other inflammatory markers that may be related to bone loss like tumor necrosis factor (TNFa) and interleukin (IL-6).
Collagen connections. Collagen support may be something you connect with joint or skin health, but there’s a bone-health element, too. “Bone consists of about 30% collagen, which forms the flexible framework giving our bones their ‘toughness’ or their flexibility to absorb impact and bend, rather than break,” states Schauch.
She adds another bonus: collagen is a binding site for bone-health minerals such as calcium and phosphorous. Therefore, Schauch believes that collagen is critical to increasing bone mass and good-quality bone.
Schauch says nutrients involved in collagen production are being studied more and more by researchers; these include vitamin C and orthosilicic acid, which is gaining increased attention. She references a 12-month study conducted on 136 women, who were either given daily calcium (1,000 mg)/D3 (20 micrograms)/choline-stabilized orthosilicic acid (ch-OSA) or a placebo (28). The researchers found the ch-OSA was beneficial for improving markers of bone formation.
States Schauch, “This study demonstrated that adding ch-OSA to a standard calcium and vitamin D supplement regimen increased the production of bone collagen 15% (measured as P1NP) and bone mineral density at the critical hip region 2% compared to just the calcium and vitamin D supplements.”
Another growing aspect of collagen support for healthy bones, she states, is using nutrients that neutralize homocysteine, which Schauch calls the “anti-collagen amino acid.” Such nutrients include choline, vitamin B6, vitamin B12 and folic acid.
Silica support. Myers says silica should be on our radars, though many women may not be aware of it. Silica, she states, “keeps the bone-building process running smoothly, bringing more calcium into the bones, allowing less calcium to leach away from the bones, but still keeping the process balanced the way nature intended. It’s the perfect choice for daily, long-term bone building.”
She feels that 30–40 mg daily helps build healthy bones. A formula from her company sources the silica from horsetail, and then blends it with a marine oil to enhance absorption. “This supplemental silica boosts calcium absorption and retention by up to 50%,” she states.
Lifestyle choices. Clouatre believes that two standouts for bone building include doing weight-bearing exercises (like walking) and eating a good diet with nutrients that support bone health.
Levin believes this includes alkaline foods. “A diet that is alkaline forming encourages bone mass while diets that cause systemic acidosis discourage bone mass,” he explains. “Whole plant foods, including fruits, are typically alkaline forming. Lists are available online of alkaline-forming foods.”
Clouatre cites a study in which an Ohio State University researcher tested whether a branded supplement plus resistance training helped bone health. “Upon comparing data from before and after the eight-week study intervention, Bone-Up treatment (but not placebo) was found to produce statistically significant changes in urinary DPD and alpha-helical peptide (markers of bone degradation), plasma bone specific alkaline phosphatase (a marker of bone synthesis), plasma 25-OH-vitamin D (an indicator of vitamin D nutritional status) and plasma parathyroid hormone (a hormone that affects bone metabolism and is affected by calcium nutritional status),” Clouatre says (29).
Inclusive approaches. Before moving on, one should consider the perspective of Mooney, who believes that bone health support works best when a combination of essential nutrients are taken in just the right potencies to build both bone mass and bone strength. “Taken together, these nutrients create a formidable bone-building team,” states Mooney.
He believes this includes calcium (1,000 mg) (30), magnesium (250–750 mg) (31), zinc (15 mg) (32), vitamin D (700-800 IU) (33), vitamin C (1,000 mg) (34), boron (3 mg) (35), manganese (5 mg), vitamin K (80 mcg) (36), copper (2.5 mg), folic acid (1,000 mg) (37) and iron (+20 mg) (38).
Note one last point raised by Badmaev: “The statistical data indicates that the more healthy bone is built in youth, the more resilient is the skeleton with aging.” Therefore, ensuring healthy bones should start in childhood.
What’s Best for Breasts?
According to the most recent statistics, 211,731 U.S. women were diagnosed with breast cancer in 2009, and 40,676 women died from the disease that same year (39). These startling numbers have women very interested in taking preventative measures to support breast health. While one’s diet and supplement regimen won’t prevent or treat any disease, there have been some interesting connections in the literature that your female clientele may want to hear more about.
Red flags: low nutrient levels. Researchers have noticed some trends in women diagnosed with breast cancer that relate to their nutrient levels.
One of the most well-known is highlighted by Avila, who tells us that women with low levels of vitamin D in their blood have a higher risk of breast cancer. In addition to helping the body absorb calcium for bone health, he believes, “Vitamin D may play a role in controlling normal breast cell growth and may be able to stop breast cancer cells from growing.”
Leong speaks of vitamin D in a different way: women who are deficient in this vital vitamin had a greater chance of being diagnosed with aggressive forms of the cancer. He states, “Women who are deficient in vitamin D (below 20 ng/ml) were eight times more likely to be diagnosed with malignant breast cancer than those with sufficient levels of vitamin D (40).”
Clouatre adds that it’s not just breast cancer with ties to D; low blood levels of vitamin D are also associated with a 30–50% increased risk of colon and prostate cancers. Vitamin D is said to have a protective effect against breast cancer (41), and “the Institute of Medicine has agreed that there are known mechanisms that suggest vitamin D does, indeed, offer some protection against cancers,” states Clouatre.
From D, we go to E deficiencies as another possible link to breast cancer. Clouatre says that the level of vitamin E in the blood has a strong correlation with breast and other cancers. “A number of studies indicated a four- or five-fold greater risk of breast cancer in those with the lowest blood vitamin E levels, whereas a few large trials have been unable to confirm this relationship.”
In studies, patients with benign breast lumps had 65% more tocotrienols (alpha-, gamma-, delta-tocotrienols) in the tumor’s tissue than those with malignant lumps (42). According to Leong, “The researcher suggested that this could be due to tocotrienols’ role ‘as a potent antioxidant in quenching free radicals and regulating peroxidation reactions.’” He says other studies on a branded palm tocotrienol complex (Tocomin from his company) found it causes cell death in breast cancer cells (43).
There’s also the B and C vitamins to worry about. According to Mooney, long-term deficiencies of vitamin B6 (44), folate (45), vitamin B12 (46) and vitamin C (47) are associated with higher rates of breast cancer.
Schauch says folic acid “helps block the division of rapidly dividing cells, such as those that occur in cancer formation,” while “vitamin B12 assists in the production of RNA and DNA, the genetic material in each cell. Vitamin B12 also assists vitamin C, which is critical for a strong immune system.” The reason why, she says, is that vitamin C builds dense connective tissue and assists the white blood cells, which, in turn, provides immune-health benefits.
Other known deficiencies in women with breast cancer have to do with diet. States Levin, “Women with the lowest levels of soy protein and isoflavones in their diet have been shown to have lower breast health rates than those with the highest consumption, with about a 30% difference.”
And Leong points out a study of Japanese women that found those who consumed a lot of iodine in their diets had a low incidence of benign and malignant breast disease (48).
Myers explains a potential reason why iodine is so helpful: “[It] helps rid the body of toxic bromide, chloride and fluoride—three iodine impostors that attach themselves to iodine receptor sites in the body and are all too common in our environment. That’s one of the many reasons that I believe it is critical that we get high levels of iodine each day.”
Also related to diet is soluble fiber intake, something that Joiner-Bey believes makes a difference in breast cancer. “Soluble fiber in the diet will sequester estrogens that the liver is trying to discard in the bile to facilitate the excretion of these hormones from the body,” he states. “This feature of soluble fiber, as found in flaxseed and chia seed, reduces estrogen load in a woman’s body, thereby reducing breast cancer risk.”
Clouatre weighs in on diet, too, noting that carotenoid consumption, particularly from a variety of fruits and vegetables, may be inversely correlated with breast cancer incidence.
“Beta-carotene and other carotenoids are very potent antioxidants that have been shown to reduce the risk of breast cancer by blocking the initiation and promotion of cancer by binding free radicals,” adds Schauch. She directs our attention to a study of 153 newly diagnosed breast cancer patients plus a 151-person control group. “The study found that women with the highest beta-carotene levels in their blood were 47% less likely to be diagnosed with breast cancer than women with the lowest levels (49),” she states.
Green light: protective effects. Many of the aforementioned supplements are recommended for their protective effects against breast cancer. Two other important nutrients to add in are omegas and lignans. According to Joiner-Bey, the omega ALA (such as that found in flaxseed oil) has been found to do something pretty amazing: turn off breast cancer genes. Meanwhile, flaxseed lignans “occupy estrogen receptors on cell membranes, thereby reducing the cell-multiplying influence of human estrogens because plant lignans have only 2% of the potency of human hormones,” states Joiner-Bey.
According to information from Sloan-Kettering, flaxseed inhibited human breast cancer growth and metastasis in mice studies because of its ability to down-regulate insulin-like growth factor I and epidermal growth factor receptor expression. It also may cause cancer cells to die off by upregulating p53 mRNA (50).
A final important natural compound to note is curcumin, which Myers states “has clearly been shown to prevent and inhibit cancer development in a number of studies.” She believes this extract is beneficial for stopping cancer cells from forming, killing existing cancer cells and stopping cancer from metastasizing. WF
References
1. http://www.factsfiguresfuture.com/issues/june-2013/in-retail,-yes,-women-are-all-that.html
2. M.G. Brush, et al., “Pyridoxine in the Treatment of Premenstrual Syndrome: A Retrospective Survey In 630 Patients,” Brit. J. Clin. Pract. 42 (11), 448-452 (1988).
3. E.R. Bertone-Johnson, et al., “Calcium and Vitamin D Intake and Risk of Incident Premenstrual Syndrome,” Arch. Intern. Med. 165 (11), 1246–1252 (2005).
4. S. Thys-Jacobs, et al., “Calcium Supplementation in Premenstrual Syndrome a Randomized Crossover Trial,” J. Gen. Intern. Med. 4 (3), 183–189 (1989).
5. R.S. London, et al., “Efficacy of Alpha-Tocopherol in the Treatment Of The Premenstrual Syndrome,” J. Repro. Med. 32 (6), 400–404 (1987).
6. F. Facchinetti, et al., “Magnesium Prophylaxsis of Menstrual Migraine: Effects on Intracellular Magnesium,” Headache 31 (5), 298–301 (1991).
7. A.F. Walker, et al., “Magnesium Supplementation Alleviates Premenstrual Symptoms of Fluid Retention,” J. Wom. Health 7 (9), 1157–1165 (1998).
8. R. Schellenberg, et al., “Treatment for the Premenstrual Syndrome With Agnus Castus Fruit Extract: Prospective, Randomized, Placebo Controlled Study,” Brit. Med. J. (20), 322, 134–137 (2001).
9. http://www.natracare.com/p26/en-GB/Your-Health.aspx
10. C.M. Dording et al., “A Double-Blind, Randomized, Pilot Dose-Finding Study of Maca Root (L. Meyenii) for the Management of SSRI-Induced Sexual Dysfunction,” CNS Neurosci. Ther. 14 (3), 182–191 (2008).
11. E. Liske, et al., “Physiological Investigation of a unique extract of black cohosh (Cimicifugae racemosae rhizoma): A 6-Month Clinical Study Demonstrates No Systemic Estrogenic Effect,” J. Women’s Health Gend. Based Med. 11 (2), 163-174 (2002).
12. J.S. Finkelstein, et al.,“Bone Mineral Density Changes during the Menopause Transition in a Multiethnic Cohort of Women,” J. Clin. Endocrinol. Metab. 93 (3), 861–868 (2008).
13. Arthritis Foundation, http://www.arthritis.org/research/funded-research/research-update/ru-march-april-2008/rate-bone-loss-menopause/
14. Armas LA, Hollis BW, Heaney RP. Vitamin D2 is much less effective than vitamin D3 in humans. J Clin Endocrinol Metab. 2004;89(11):5387-5391.
15. Deroisy R, Zartarian M, Meurmans L, et al. Acute changes in serum calcium and parathyroid hormone circulating levels induced by the oral intake of five currently available calcium salts in healthy male volunteers. Clin Rheumatol 1997;16(3):249‑53.
16. Hansen C, Werner E, Erbes HJ, Larrat V, Kaltwasser JP. Intestinal calcium absorption from different calcium preparations: influence of anion and solubility. Osteoporos Int 1996;6(5):386-393.
17. Gonnelli S, Cepollaro C, Camporeale A, Nardi P, Rossi S, Gennari C. Acute biochemical variations induced by two different calcium salts in healthy perimenopausal women. Calcif Tissue Int 1995;57(3):175‑7.
18. Harvey JA, Zobitz MM, Pak CY. Dose dependency of calcium absorption: a comparison of calcium carbonate and calcium citrate. J Bone Miner Res 1988;3(3):253‑8.
19. Wood RJ, Serfaty‑Lacrosniere C. Gastric acidity, atrophic gastritis, and calcium absorption. Nutr Rev 1992;50(2):33‑40.
20. Valente M, Bufalino L, Castiglione GN, et al. Effects of 1-year treatment with ipriflavone on bone in postmenopausal women with low bone mass. Calcif Tissue Int 1994;54:377-80.
21. Agnusdei D, Camporeale A, Gonnelli S, et al. Short-term treatment of Paget’s disease of bone with ipriflavone. Bone Miner 1992;19 Suppl 1:S35-42.
22. Melis GB, Paoletti AM, Cagnacci A, et al. Lack of any estrogenic effect of ipriflavone in postmenopausal women. J Endocrinol Invest 1992;15:755-61.
23. Chen YM, Ho SC, Lam SS, et al. Soy isoflavones have a favorable effect on bone loss in Chinese postmenopausal women with lower bone mass: a double-blind, randomized, controlled trial. J Clin Endocrinol Metab 2003;88:4740-7.
24. Shedd-Wise KM, Alekel DL, Hofmann H, Hanson KB, Schiferl DJ, Hanson LN, Van Loan MD. The soy isoflavones for reducing bone loss study: 3-yr effects on pQCT bone mineral density and strength measures in postmenopausal women. J Clin Densitom. 2011 Jan-Mar;14(1):47-57.
25. Taku K, Melby MK, Takebayashi J, Mizuno S, Ishimi Y, Omori T, Watanabe S. Effect of soy isoflavone extract supplements on bone mineral density in menopausal women: meta-analysis of randomized controlled trials. Asia Pac J Clin Nutr. 2010;19(1):33-42.
26. Aktifanus AT, et al. 2012
27. P. Lencel and D. Magne, “Inflammaging: The Driving Force in Osteoporosis?” Med. Hypotheses. 76 (3), 317–321 (2011).
28. T.D. Spector et al., “Choline-stabilized Orthosilicic Acid Supplementation as an Adjunct to Calcium/Vitamin D3 Stimulates Markers of Bone Formation in Osteopenic Females: a Randomized, Placebo-Controlled Trial,” BMC Musculoskeletal Disorders, 9 (85), 2008.
29. (Nutritional & Environmental Medicine 2007;16(1):26 - 32)
30. Storm D, et al. Calcium supplementation prevents seasonal bone loss and changes in biochemical markers of bone turnover in elderly New England women: a randomized placebo-controlled trial. Clin Endocrinol Metab. 83(11):3817-25 1998 Nov.
31. Stendig-Lindberg G, et al. Trabecular bone density in a two year controlled trial of peroral magnesium in osteoporosis. Magnesium Res. 1993 Jun;6(2):155-63.
32. Strause L, et al. Spinal bone loss in postmenopausal women supplemented with calcium and trace minerals. J Nutr. 1994 Jul;124(7):1060-4.
33. Bischoff-Ferrari H, et al. Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. JAMA. 2005 May 11;293(18):2257-64.
34. Morton DJ, et al. Vitamin C supplement use & bone mineral density in postmenopausal women. J Bone Min Res. 2001, 16:135-140.
35. Nielsen FH, et al. Effect of dietary boron on mineral, estrogen, and testosterone metabolism in postmenopausal women. FASEB Journal. 1987 Nov;1(5):394-7.
36. Schaafsma A, et al. Vitamin D3 and vitamin K1 supplementation of Dutch postmenopausal women with normal and low bone mineral densities: effects on serum 25-hydroxyvitamin D and carboxylated osteocalcin. Euro J Clin Nutr. 2000;54:626.
37. Cagnacci A, et al. Relation of folates, vitamin B12 and homocysteine to vertebral bone mineral density change in postmenopausal women. A five-year longitudinal evaluation. Bone. 2008 Feb;42(2):314-20. Epub 2007 Nov. 12.
38. Harris MM, et al. Dietary iron is associated with bone mineral density in healthy postmenopausal women. J Nutr. 133;3598-3602, 2003.
39. http://www.cdc.gov/cancer/breast/statistics/
40. (Steck S, et al., 2010)
41. Today’s Dietician 2012;14,10:58
42. Nesaretnam K, et al., 2007
43. (Paul W Sylvester & Sumit Shah, 2002), inhibit proliferation of malignant breast cancer cells (Samant GV, et al., 2010).
44. Lurie G, et al. Prediagnostic plasma pyridoxal 5’-phosphate (Vitamin b6) levels and invasive breast carcinoma risk: the multiethnic cohort. Cancer Epidemiol Biomarkers Prev. 2012 Nov;21(11):1942-8. doi: 10.1158/1055-9965.EPI-12-0717-T. Epub 2012 Aug 9.
45. Rohan TE, et al. Dietary folate consumption and breast cancer. JNCI (2000) 92(3):266-269. doi: 10.1093/jnci/92.3.266
46. Yang D, et al. Dietary intake of folate, B-vitamins and methionine and breast cancer risk among Hispanic and non-Hispanic white women. PLoS One. 2013;8(2):e54495. doi: 10.1371/journal.pone.0054495. Epub 2013 Feb 11.
47. Adzersen KH, et al. Raw and cooked vegetables, fruits, selected micronutrients, and breast cancer risk: a case-controlled study in Germany. Nutr Cancer. 2003;46(2):131-7.
48. LeMarchand L. Kolonel LN, Nomura AM., 1985
49. Ching, S.D. et al. J Nutr. 2002
50. Sloan-Kettering, “Flaxseed,” www.mskcc.org/cancer-care/herb/flaxseed
Published in WholeFoods Magazine, October 2013











