Part One of a Five-Part Series on Heart Health
In the United States, heart disease is responsible for nearly one in four deaths each year (1). It’s a given that taking care of the heart is one of the most important things a person can do to ensure good health throughout life. But, how to do so from a nutritional standpoint is a complex topic, and one that deserves our attention.
This month, WholeFoods Magazine kicks off its five-part series on heart health by focusing on cholesterol. In the coming months, we will tackle blood pressure, support for those on statins, homocysteines and heart-healthy foods. We hope this in-depth look at the many facets of heart health will help you keep your shoppers’ tickers in tip-top shape for years to come.
A Two-Faced Issue
From an early age, we are taught to limit cholesterol intake and keep our “bad” cholesterol levels as low as possible. But, a new wave of thinking is challenging this mindset.
“Say ‘cholesterol’ and the first thing that comes to mind is heart disease. Very few compounds have been vilified as much. As a result, many popular, but wrong and even dangerous, myths have developed,” says Andreas M. Papas, Ph.D., adjunct professor at Quillen College of Medicine, East Tennessee State University, Johnson City, TN.
Before addressing the controversies, retailers should understand that there is not consensus on whether focusing on bad cholesterol for heart health is warranted. Some of your shoppers may be on statin drugs to lower cholesterol and need nutritional support. Others may want to supplement to keep levels healthy and some may not want to focus on cholesterol at all. A retailer should be ready to help all shoppers find the nutritional support that best meets their needs for heart health.
The Building Blocks
Cholesterol is a waxy substance that cells use to produce hormones and vitamin D. Plus, says Papas, “The liver uses cholesterol to make bile acids, which are essential for digestion and absorption of lipids and fat-soluble vitamins including vitamin E.”
It’s easy to see that the body produces cholesterol for a reason; we need it. States Duane Graveline, M.D., M.P.H., author of three books on statin effects and author of www.spacedoc.com, “The entire memory function of our brains, the formation and function of memory synapses, is so dependent upon cholesterol that special cholesterol-producing cells known as glial cells are charged with the task of producing cholesterol upon demand.” The average healthy person will make all the cholesterol he or she needs, but it is also present in many foods.
When our cholesterol levels are tested, results are often viewed as triglycerides (VLDL), low-density lipoproteins (LDL or “bad”) and high-density lipoproteins (HDL or “good”). Lipoproteins are fat–protein packages that carry cholesterol through our bloodstream. For instance, HDL brings cholesterol to the liver for removal (hence, it’s seen as good).
 LDL cholesterol is considered “bad,” even though it does some important jobs. The reason why is that some say in excess, it can accumulate in the arteries, blocking them and causing atherosclerosis and stroke.
LDL cholesterol is considered “bad,” even though it does some important jobs. The reason why is that some say in excess, it can accumulate in the arteries, blocking them and causing atherosclerosis and stroke.
LDL cholesterol may be even more of a problem when it oxidizes. In fact, as we’ll flesh out later, health authorities are beginning to believe oxidation (and the damage it causes) may be a better indicator of future heart disease than the LDL number itself.
“Oxidized LDL can create inflammation in your arteries and increase the risk of a heart attack or stroke,” Jeremy Bartos, Ph.D., senior product development manager at ChromaDex, Inc., Irvine, CA, states. “Over time, this causes the formation of plaques, which can restrict the flow of blood and lead to strokes, heart attacks, and other coronary heart diseases.” To deal with this issue, he suggests that one decrease the body’s free radical load by taking antioxidants such as pterostilbenes from blueberries.
But traditionally, the focus has been on the numbers, not oxidation. Total cholesterol should be 200 mg/dl or less for most people (and even lower for those at risk of heart problems), health authorities feel. A score of 100 mg/dl for LDL is considered optimal for most people, and some believe levels as low 60 mg/dl is even better (2). Essentially, the lower the LDL the better has been the mantra repeated by many physicians and health specialists (2).
Many people believe otherwise.
Problem 1: Relying on LDL to Predict Heart Disease
For one, Jacob Teitelbaum, M.D., medical director of the national Fibromyalgia and Fatigue Centers and Chronicity, author and nutrition authority, feels we shouldn’t place too much stock in these numbers. “The reason it gets attention is that it is easy to test for and results in ~$29 billion/year in (largely unhelpful) sales of prescription medications,” he states.
Putting the situation bluntly is author Jonny Bowden, Ph.D., C.N.S., aka “The Rogue Nutritionist,” and scientific advisory board member at Barlean’s, Ferndale, WA. He states, “We’re finding that cholesterol is a very bad predictor of heart disease—half the people who have heart attacks have perfectly normal cholesterol and half the people with ‘elevated’ cholesterol have perfectly healthy hearts.”
The reason why, says Dallas Clouatre, Ph.D., R&D consultant to Jarrow Formulas, Los Angeles, CA, is that “the value of reducing both total cholesterol and LDL-C appears to be significant only if one looks at lowering these ‘markers’ rather than at all meaningful clinical endpoints.” He points to a study published last year. The researchers found the risk of major heart events in those taking statins for high cholesterol is only reduced by one-third! Thus, concentrating on lowering LDL could be missing the mark (3).
The water becomes muddier when we consider all causes of death. In this case, Clouatre feels triglycerides and HDL counts are more meaningful a predictor than total and LDL cholesterol. He says, “the greatest overall health and longevity is found with a total serum cholesterol reading of approximately 200 to 240 mg/dL.” Again, many health professionals work under the rubric that total cholesterol should be less than 200 mg/dL.
Another point to consider comes from Steve Holtby, president and CEO, Soft Gel Technologies, Inc., Los Angeles, CA. He says cholesterol particles’ size is an important factor for determining cardiovascular risks. The smaller the size, the better the chance it can enter arterial walls and cause damage.
Teitelbaum even makes the case that high cholesterol may be more indicative of non–heart-related problems. “When I see high cholesterol, it tells me to consider treating for an underactive thyroid (even if tests are normal), to have the person cut down excess sugar and, in men, to treat for low testosterone (a major cause of metabolic syndrome and high cholesterol) using bioidentical hormones,” he states.
So, how can we make sense of this new message? LDL is just one number and there are many factors to consider in maintaining the heart.
Problem 2: Glossing over HDL and Triglycerides
Thus, when we consider getting cholesterol levels in a healthy range, remember HDL. Papas reminds us, “HDL is known as good cholesterol because a high level of HDL seems to protect against heart attack. This is the reason why high HDL brings an approving smile from our doctor. We may escape the stern lecture even if our LDL is a tad above normal,” he states.
 High HDL levels are even associated with positive health factors outside the cardiovascular arena like reduced rates of cancers and of neurodegenerative and neurovascular diseases (4).
High HDL levels are even associated with positive health factors outside the cardiovascular arena like reduced rates of cancers and of neurodegenerative and neurovascular diseases (4).
Unfortunately, few shoppers differentiate between HDL and LDL cholesterol, “so the healthy lifestyle retailer needs to do this,” states Dean Mosca, president of Proprietary Nutritionals Inc., Kearny, NJ. “The best way is creative, simple and eye-catching signage and through the retailer’s social media (such as Facebook and Twitter).”
This could entail encouraging community members to post their personal stories about changes made in the right direction. “Many people should be willing to do this, as achieving healthier cholesterol levels is something most folks feel great and prideful about. And, you will be building a community that will be active with one another, which should also translate into new sales as well as stronger loyalty,” says Mosca.
The other angle is triglycerides. Researchers believe an excess of triglycerides contributes to atherosclerosis, or hardening/thickening of the arteries (5). Thus, keeping these levels in check is an important way to support a healthy cardiovascular system.
Problem 3: Forgetting Too-Low LDL Is a Problem
Striving for ultra-low cholesterol levels could be dangerous. As noted previously, Craig Klein, M.S., L.N., C.N.S., Michael’s Naturopathic Programs, San Antonio, TX, reminds us, “Cholesterol has vital functions in our bodies that impact many areas of our health…If there was a special magnet that could pull all of the cholesterol out of a person’s body, that person would be in trouble.”
States Gary Walker, president of Sylvan Bio, Inc., Kittanning, PA, “Your liver makes about 75% of your body’s cholesterol, which is an indication of its importance. Therefore, it is important to understand that too little can be at least as damaging as too much.”
Bowden agrees, and adds this surprising fact: low cholesterol is associated with as many or more risks than high cholesterol. These include higher rates of cancer and infectious disease.
Adding to the list of negative health problems from low LDL is Michael Smith, M.D., staff doctor with Life Extension, Fort Lauderdale, FL. “If you significantly lower a man’s cholesterol, his testosterone levels can drop. This loss of testosterone is a risk factor for heart disease,” he says. “So basically, you trade one risk factor for another.”
Too-low cholesterol could even be induced by prescriptions. Trisha Sugarek MacDonald, B.S., M.S., director of research & development/national educator for Bluebonnet Nutrition Corporation, Sugar Land, TX, states, “There is also the possibility of the unexpected and unexplained relationship between low levels of cholesterol (i.e., less than 160 mg/dL), whether natural or therapeutically lowered (i.e., statin use), and adverse psychological and behavioral effects, particularly in the arena of mood and anxiety disorders.”
Sugarek MacDonald highlights an interesting study linking cholesterol-lowering methods (like diet and pharmaceuticals) with an increased chance of death from accidents, suicide or violence (6). States Sugarek MacDonald, “This research has spurred an all-out investigation—the idea of identifying a biological marker for schizophrenia, other mood disorders (i.e., bipolar disorder, major depression) or suicidality is of the utmost importance. More studies are needed to clearly identify the correlation of cholesterol levels with mood, risk for suicide, and the biochemistry of serotonin.”
 And, Jolie Root, nutritionist for Carlson Laboratories. Arlington Heights, IL, adds, “Very low cholesterol is linked to depression and poor health outcomes, including increased risk of dying sooner in the elderly.”
And, Jolie Root, nutritionist for Carlson Laboratories. Arlington Heights, IL, adds, “Very low cholesterol is linked to depression and poor health outcomes, including increased risk of dying sooner in the elderly.”
Even pregnant women can have problems (preterm birth and low birth weight) if their LDL levels are too low, according to Bartos.
So, how low does cholesterol need to drop before it’s a problem? In many cases, less than 160 mg/dL. Now remember, an “optimal” level, according to the medical community, is less than 200 mg/dL.
Thus, given the importance of both kinds of cholesterol, Bowden says our notion of “good” and “bad” cholesterol is “completely outdated.” There are five different types of LDL cholesterol, all of which behave differently in the body. Says Bowden, “Some ‘bad’ cholesterol (LDL-pattern A) is actually harmless.”
Problem 4: Statins can cause Health Problems
In many individuals, statin drugs cause problems they never bargained for. Says Smith, “Cholesterol-lowering medications are now associated with dementias and even metabolic problems like diabetes.”
Michael T. Murray, N.D., director of product development and education at Natural Factors, Everett, WA, says statin drugs decrease mortality, hospitalizations and cardiovascular events, however “the debate remains whether statin therapy represents the optimal treatment approach to primary prevention of coronary artery disease in patients with the only risk factor being elevated LDL.”
He adds a startling statistic: “In 2011, it is estimated that more than one of every six adults—nearly 40 million people—were taking a statin drug to lower LDL. Therefore, the focus for many will be on the support of statin therapy.”
Part three of this series will deal with this issue in depth, but for now, advise shoppers to take supplements with CoQ10 (ubiquinone or ubiquinol), since their medication could be stopping the body from making this important nutrient. Omega-3s, tocotrienols and vitamin D3 are also important choices.
Diet and the “Demon”
The demonization of cholesterol has strongly influenced our diets to the point that eating an egg—complete with the yolk—is a decadency. “It should be noted that the effect of diet on blood cholesterol levels varies from person to person,” says Walker. So, some feel an all-out ban on dietary cholesterol isn’t warranted.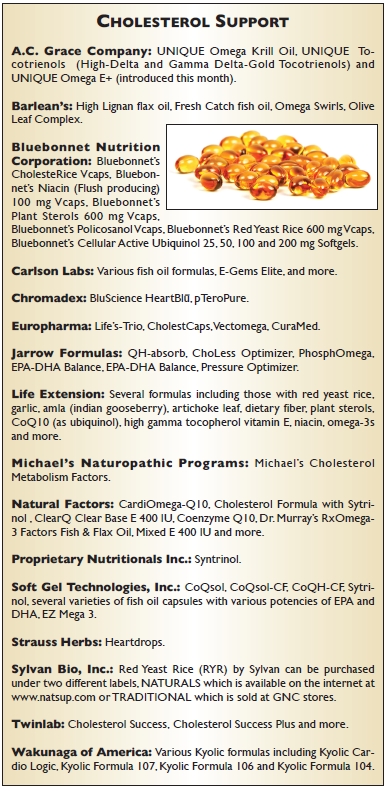
It is a myth that diet controls cholesterol levels, according to Papas. The liver makes about 80% of our cholesterol daily (one gram), leaving only about 20% up to diet. “Sure, the amount of fat and cholesterol we eat may influence all blood lipids, including cholesterol,” he states. “But in order to maintain a healthy cholesterol profile, we need to influence the main source: the cholesterol produced in our liver and how much is cleared.” Papas says genes play a major role in this process, as can lifestyle choices.
Age is a factor, too, according to Smith: “One reason for this over-production by the liver is the loss of hormones that comes with age. The liver up-regulates cholesterol production so you can maintain healthy hormone levels.” Thus, someone who may never have had cholesterol “problems” before may see their numbers climb even if diet isn’t altered.
So, is stripping eggs from the diet the answer to heart health? Holtby says that “the 2010 Dietary Guidelines for Americans support the role of eggs in a healthy diet. The policy report states that healthy individuals can enjoy an egg daily and suggests an egg a day does not result in increased blood cholesterol levels.”
The issue of withholding dietary sources of cholesterol from his family for 20 years is enough to make Graveline (a physician) “seethe with anger.” He states, “I must have written 10,000 prescriptions for cholesterol-lowering drugs to my often skeptical patients and now we find that cholesterol-lowering is not how these statin drugs achieve their benefit.”
This is an important point. “Statin benefit comes from its effect on underlying antioxidative and inflammatory processes that we only now are beginning to understand. Cholesterol reduction has nothing to do with it,” Graveline states.
Some shoppers may not be ready to jump on board with the idea of bringing cholesterol back into the diet. For them, says Bartos, “The best way for a healthy person to handle dietary intake of cholesterol is to work closely with their doctor to determine the risk of ingesting larger amounts of cholesterol.”
Those in favor of the American Heart Association’s advice should limit daily intake of cholesterol to below 300 mg. “One egg contains about 200 mg of cholesterol. Therefore, it is important to look for and consume healthier options that contain the nutrients found in the high-cholesterol foods,” says Klein, adding that cholesterol is primarily found in animal-based foods.
 Smith sums it up by stating: “It looks like the old saying, ‘Everything in moderation,’ is really true. You can enjoy eggs; just don’t overdo it.”
Smith sums it up by stating: “It looks like the old saying, ‘Everything in moderation,’ is really true. You can enjoy eggs; just don’t overdo it.”
Consumers worried about dietary cholesterol should also consider cutting down on sources of saturated and trans-fats such as processed and packaged foods.
The Role of Supplementation
Supplements can’t claim to lower cholesterol, but they can support healthy levels in important ways. Some customers may choose to focus on limiting oxidized LDL cholesterol, while others may want to get their triglyceride or HDL numbers as healthy as possible. Still others may follow the traditional advice of keeping LDL cholesterol in check. Rest assured; your store can handle all these needs.
Oxidized LDL and inflammation. We previously discussed why oxidized LDL could be as (or more) important than the LDL number alone. Remember, oxidized LDL can cause inflammation in the arteries and, according to Graveline, “Inflammation has been implicated in cardiovascular disease. [It] has been found to participate in all phases of the atherosclerotic process.”
One way physicians check for inflammation is by looking at C-reactive protein (CRP); high levels seem correlated with heart disease risk. Graveline speaks of the JUPITER study in which 18,000 healthy men and women with cholesterol levels of 130 or less were studied. All had modestly elevated CRP levels and were either given a statin or a placebo. According to Graveline, “After 19 months of observation, the ethics committee insisted the study be stopped because of the appearance of excess numbers of heart attacks and strokes in the control group. This study demonstrated convincingly that cholesterol level is irrelevant to cardiovascular risk determination.” Rather, inflammation (measured by CRP levels) is a better marker for risk.
Graveline states that tocotrienols from vitamin E have unique anti-inflammatory effects that are similar to how statins work. But, the vitamin must be taken properly, since tocotrienols can be converted to alpha-tocopherol in the body, and taking large amounts of tocotrienols could reduce their anti-inflammatory effect. “Ordinarily 80–100 mg of annatto tocotrienol (90% delta and 10% gamma) taken daily has the maximum desirable effect,” Graveline states.
Bartos agrees antioxidants are key to the cholesterol-support category. He says, “Polyphenols are well known for their antioxidant potential, which in part comes from the free hydroxyl groups that act as the electron donors.” For this reason, he zeros in on blueberry-derived pterostilbenes.
Olive leaf extract also may be in a unique position to reduce levels of oxidized LDL. The reason has to do with its hydroxytyrosol content, which was shown to reduce oxidized LDL cholesterol (7).
A study produced positive results for olive polyphenols. In a three-week rotation, 200 healthy men were given 25 mL/day of olives with varying phenolic content. Blood levels of oLAB (i.e., antibodies to LDL cholesterol that help protect the arteries when LDL is oxidized ) were tested. Overall, “Olive oil phenolic content increased oLAB generation, with the effect being stronger at higher concentrations of oxLDL (p = 0.020 for interaction)” (8).
According to the University of Texas Southwestern Medical Center in Dallas, guggul aids cholesterol metabolism and offers antioxidant benefits, “which supports the normal oxidation levels of cholesterol in the body,” according to information on the Himalaya Herbal Healthcare Web site.
Also noted for anti-inflammation and antioxidant properties are artichoke extract, CoQ10, vitamin D and potassium. Regarding the latter, “Potassium helps prevent free-radical damage to the walls of blood vessels and arteries, which in turn, can prevent inflammation and LDL cholesterol oxidation,” says Cheryl Myers, chief of scientific affairs for EuroPharma, Green Bay, WI.
Triglycerides. Triglyceride support is another way supplements can keep the heart healthy. “Omega-3s keep arteries and blood vessels flexible, and protects the cell structures of hearts, too,” adds Myers.
 Omega-3s are said to benefit triglyceride levels and protect against cardiovascular disease (CVD). The dosages vary for these two applications. States Murray, “for preventive effects against CVD, the dosage recommendation is 1,000 mg EPA+DHA per day, but for lowering triglycerides the dosage is 3,000–5,000 mg EPA + DHA. The degree of reduction in triglycerides with fish oil is on par with other drug therapies.” A dose of 250 mg per day of EPA and DHA may be a minimum target for healthy individuals to achieve cardiovascular health (9).
Omega-3s are said to benefit triglyceride levels and protect against cardiovascular disease (CVD). The dosages vary for these two applications. States Murray, “for preventive effects against CVD, the dosage recommendation is 1,000 mg EPA+DHA per day, but for lowering triglycerides the dosage is 3,000–5,000 mg EPA + DHA. The degree of reduction in triglycerides with fish oil is on par with other drug therapies.” A dose of 250 mg per day of EPA and DHA may be a minimum target for healthy individuals to achieve cardiovascular health (9).
Clouatre offers some study backing for this use:
• In a 14-year prospective study on 45,000+ men, consuming at least 250 mg of EPA and DHA daily reduced the risk of sudden cardiac death by 40–50% (10).
• Those consuming the highest levels of omegas had 50% less risk of congestive heart failure than others (11).
Another benefit is omega-3s’ effect on particle size. Again, smaller particle sizes of LDL could increase arterial damage. Says Root, “EPA and DHA omega-3s increase particle size of both HDL and LDL reducing the rate of atherogenic damage to blood vessels.”
HDL. For HDL support (and other cholesterol benefits), consider introducing clients to policosanol. Sugarek MacDonald explains, ”These long-chain alcohols or fatty alcohols, which mainly include octacosanol, are solid waxy substances and are soluble in water. Policosanol may help maintain healthy lipid levels.” Smith adds that it binds cholesterol in the intestines.
A literature review concluded that at doses of 10–20 mg per day, policosanol lowered total cholesterol by 17–21% and LDL by 21–29%, and raised HDL by 8–15% (12), according to Holtby. In another study, policosanol went head to head with a stain drug (lovastatin) (13). The authors found, “Policosanol significantly (p < 0.001) lowered total cholesterol (TC) and low-density lipoprotein-cholesterol (LDL-C) by 17.5% and 31.0%, respectively, and meanwhile increased (p < 0.01) high-density lipoprotein-cholesterol (HDL-C) levels by 31.5%. Lovastatin reduced (p < 0.01) TC (18.0%), LDL-C (22.6%), and (p < 0.05) triglycerides (9.8%)”.
Also key for HDL support are citrus polymethoxylated flavones (PMF) such as one branded form that also combines tocotrienols (Sytrinol).
Mosca speaks of a 10-subject trial in which those with high cholesterol were given 300 mg of Sytrinol daily for a month. In the end, the ingredient lowered total cholesterol by 20%, apolipoprotein B (a component of LDL) by 21% and triglycerides by 28%. Of note, apolipoprotein A1 increased 5%, which is good news because it’s a structural protein found in HDL cholesterol. “The best news is Sytrinol worked independent of diet changes,” says Mosca.
Also on the anti-inflammation front, Myers uses her company’s amla supplement as an example: “CholestCaps has been shown in two pilot clinical trials to increase HDL cholesterol—‘good’ cholesterol—levels and reduce CRP levels. It’s a great two-front approach to healthy cholesterol management, because boosting HDL by even 1% can have a significant impact. Indian gooseberry has been shown to raise them by an average of 14%.”
The B-vitamins, especially niacin, have a long history for cholesterol support. According to Murray, its benefits are two-fold: “Niacin typically lowers LDL-cholesterol levels by 16% to 23% while raising HDL-cholesterol levels by 20% to 33%. These effects, especially the effect on HDL, compare quite favorably to conventional cholesterol-lowering drugs.” Niacin has been studied for its ability to lower CRP levels and other markers of inflammation, too.
Meanwhile, Sugarek MacDonald discusses pantethine or vitamin B5, which she says supports healthy lipid metabolism.
LDL. For shoppers that want to concentrate on keeping LDL cholesterol within a healthy range, pterostilbenes may help since they “activate a protein called PPAR-alpha, which when activated inhibits the cellular processes that make LDL cholesterol and triglycerides, effectively reducing the native cholesterol load,” says Bartos.
Phytosterols are also a key player in the heart health category because they block the absorption of dietary cholesterol. Explaining how is Myers: “They move in and take over the sites in the intestines where cholesterol would be absorbed. The reason they can do this is that they are shaped so much like cholesterol that they fit perfectly into the ‘parking places’ that cholesterol would normally absorb through. Because the cholesterol has nowhere to go to be absorbed, it continues through the digestive system,” she states.
Murray states that a 41-trial meta-analysis indicated two grams of stanols or sterols may reduce LDL by 10%. “Taking higher dosages added little additional benefit,” he adds, especially in combination with foods low in saturated fat and cholesterol. And, Holtby references two other studies: “Clinical studies demonstrated that phytosterols have the ability to lower serum total cholesterol by 10–15% and LDL-cholesterol by up to 20% (14)…In 16 recently published human studies that used phytosterols to reduce plasma cholesterol levels in a total of 590 subjects, phytosterols therapy was accompanied by an average 10% reduction in total cholesterol and 13% reduction in LDL cholesterol levels (15).”
FDA is also impressed with data behind phytosterols for heart health. Holtby states, “FDA recently authorized a claim that would allow food manufacturers to label phytosterols-enriched foods with the assertion that they may reduce the risk of coronary heart disease when combined with a diet low in cholesterol and saturated fats (16).”
Flaxseed is an example of a grain rich in phytosterols, plus alpha-linolenic acid, lignans and soluble fiber. In one study, postmenopausal women not on hormone replacement therapy ate either 40 g of ground flaxseed or a control wheat for three months. In all “Flaxseed supplementation lowered both serum total cholesterol and LDL cholesterol by 6%, whereas the comparative control regimen had no such effect (17),” states Holtby. Flax is, of course, rich in omega-3s, which supports healthy arteries and blood vessels.
Soluble fiber known as beta-glucans from mushrooms, yeast, oats and barley can’t be overlooked for heart health since they help block cholesterol absorption. Since 1997, foods containing three grams of oat bran have been allowed by FDA to claim to reduce cholesterol, illustrating their importance.
Before moving on, one should emphasize that while fiber is key for heart health, not all sources of fiber offer the same benefit, according to Murray. “The greater the degree of viscosity or gel-forming nature, the greater the effect of a particular dietary fiber has on lowering cholesterol levels.”
Thus, shoppers may want to hear about new, highly viscous, soluble fiber blends (like PolyGlycopleX or PGX), because they are said to be better than single fibers for cholesterol support.
A familiar face in the cholesterol-support category is red yeast rice. This fungus makes compounds that inhibit HMG-CoA, the enzyme the liver uses to make cholesterol. Statins are HMG-CoA inhibitors, too.
According to Murray, “The development of statin drugs owe their origin to red yeast (Monascus purpureus) fermented on rice.” The natural supplement contains compounds called monacolins such as lovastatins. He states, “The marketing of an extract of red yeast fermented on rice standardized for monacolin content as a dietary supplement in the United States caused controversy in 1997 because it contained a natural source of a prescription drug. The U.S. Food and Drug Administration eventually ruled that red yeast rice products could only be sold if they were free of monacolin content.”
One trial found participants that received 2,400 mg of this supplement daily (and no cholesterol-lowering drugs) experienced a 16% reduction of total cholesterol and 22% reduction in LDL cholesterol after three months (18). Red yeast rice may also benefit triglyceride levels and endothelial inflammation.
Tocotrienols, previously mentioned for anti-inflammation, may also support healthy cholesterol levels. States Clouatre, “These members of the vitamin E family, especially gamma- and delta-tocotrienols, reduce triglycerides, reduce cholesterol synthesis and may increase receptor-mediated (liver) re-uptake of LDL.”
Many people believe the heart loves garlic for its ability to “affect the process of atherosclerosis at so many steps,” says Murray. He explains that garlic may lower total cholesterol levels, decrease LDL, increase HDL and lower triglyceride levels.
Last, the B-vitamins come up again for LDL support, specifically pantethine. In one study, a placebo or the vitamin was given to 120 people with low to moderate risk of heart disease. The pantethine group received the vietam at 600 mg/d for two months and then 900 mg/day for two months.
Overall, the authors state, "pantethine demonstrated significant (P b .005) and sustained reductions (from baseline to week 16) in total cholesterol (6 mg/dL, 0.16 mmol/L, 3%), LDL-C (4 mg/dL, 0.10 mmol/L, 4%), and apolipoprotein B (4 mg/dL, 0.04 g/L, 5%)" (19).
In an interview with the lead author, John A. Rumberger of The Princeton Longevity Center, explained what may have caused this effect (20): pantethin and a byproduct of its metabolism in the body work together to inhibit two enzymes (acetyl-CoA carboxylase and HMG-CoA) that affect triglyceride synthesis and LDL metabolism. "Pantethine increases CoA levels in cells, and favorably modifies lipoprotein metabolism. Pantethine has a mild anti-platelet aggregation property as well, which can also modify the membrane fluidity of cells and platelets. These multiple mechanisms of action can contribute to the effects of Pantethine in decreasing CVD risk," he states. WF
This heart health series is sponsored by
References
1. Centers for Disease Control and Prevention, “Heart Disease Facts,” www.cdc.gov/heartdisease/facts.htm, accessed Apr. 26, 2012.2. Cleveland Clinic, “Heart and Vascular Health & Prevention,” http://my.clevelandclinic.org/heart/prevention/cholesterol/cholesterolguidelines9_01.aspx, accessed Apr. 26, 2012.
3. P. Barter, “Raising HDL-C Can Be Achieved by Both Lifestyle Changes and Pharmacological Means. Introduction,” Atheroscler. Suppl. 12 (3), 265–266 (2011).
4. D. McGrowder et al., “The Role of High-Density Lipoproteins in Reducing the Risk of Vascular Diseases, Neurogenerative Disorders, and Cancer,” Cholesterol. (2011) 496925 (2011).
5. Mayo Clinic, “Triglycerides: Why Do They Matter?” www.mayoclinic.com/health/triglycerides/CL00015, accessed Apr. 27, 2012.
6. M.F. Muldoon, S.B. Manuck and K.A. Matthews, “Lowering Cholesterol Concentrations and Mortality: A Quantitative Review of Primary Prevention Trials,” BMJ. 301 (6747), 309–314 (1990).
7. M. Vazquez-Velasco, et al., “Effects of Hydroxytyrosol-Enriched Sunflower Oil Consumption on CVD Risk Factors,” Br. J. Nutr. 105 (10), 1448–1452 (2010).
8. O. Castañer, et al., “The Effect of Olive Oil Polyphenols on Antibodies against Oxidized LDL. A Randomized Clinical Trial,” Clin. Nutr. 30 (4), 490–493 (2011).
9. K. Musa-Veloso, “Impact of Low V. Moderate Intakes of Long-Chain N-3 Fatty Acids on Risk of Coronary Heart Disease,”Br. J. Nutr. 106 (8), 1129–1141 (2011).
10. D. Mozaffarian et al., “Interplay Between Different Polyunsaturated Fatty Acids and Risk of Coronary Heart Disease in Men,” Circulation 111 (2), 157-164 (2005)
11. D. Mozaffarian et al., “Circulating Long-Chain ω-3 Fatty Acids and Incidence of Congestive Heart Failure in Older Adults: The Cardiovascular Health Study,” Ann. Intern. Med. 155 (3), 160–170 (2011).
12. I. Gouni-Berthold and Berthold HK. “Policosanol: Clinical Pharmacology and Therapeutic Significance of a New Lipid-Lowering Agent,” Am. Heart J. 143, 356 (2002).
13. G. Castano et al., “Effects of Policosanol and Lovastatin with Intermittent Claudication: A Double-Blind Comparative Pilot Study,” Angiology 54,25 (2003).
14. T.A. Miettinen, “Stanol Esters in the Treatment of Hypercholesterolemia,” Eur. Heart J. 1 (Suppl S), S50–S57 (1999), H. Gylling, Studies of Plant Stanol Esters in Different Patient Populations,” Eur. Heart J. 1 (Suppl S), S109 (1999).
15. W.H. Ling and P.J. Jones, “Dietary Phytosterols: A Review of Metabolism, Benefits and Side Effects, Life Sci. 57, 195 (1995).
16. 65 Fed. Reg. 54685 (2090) (codified at 21 CFR [ss] 101)
17. E.A. Lucas et al., “Flaxseed Improves Lipid Profile Without Altering Biomarkers of Bone Metabolism in Post-Menopausal Women,” J. Clin. Endocrinol. Metab. 87, 1527 (2002).
18. D. Heber et al., “Cholesterol-Lowering Effects of a Proprietary Chinese Red-Yeast-Rice Dietary Supplement,” Amer. J. Clin. Nutr. 69, 231 (1999).
19. J.A. Rumberger, "Pantethine, a derivative of vitamin B5 used as a nutritional supplement, favorably alters low-density lipoprotein cholesterol metabolism in low– to moderate–cardiovascular risk North American subjects: a triple-blinded placebo and diet-controlled investigation," Nutr.Res. 31 608–615 (2011).
20. Materials supplied by Kyowa Hakko, USA.
Published in WholeFoods Magazine, June 2012