Getting sick is the pits. Life becomes even stormier if the ailment is digestion related. What’s worse is having a chronic condition of this type, which can make enjoying life’s simplest pleasures a harrowing experience. Unfortunately, many Americans are plagued by such conditions and too few have found viable options for making them feel better.
For instance, chronic, autoimmune conditions like Crohn’s disease and ulcerative colitis (so-called inflammatory bowel diseases [IBD]) are usually medicated with high-doses of steroids, chemotherapeutics, immune suppressants and other hardcore drugs that have the potential to cause serious problems like liver damage and blood toxicity. Such medications aren’t cures; individuals suffering from these and other chronic conditions are often on medications their entire lives. So many Americans rely on drugs to keep IBD in check that the market for these diseases is expected to grow by more than 60% to $5.6 billion before 2019, according to market analyst Datamonitor (1).
While natural medicine and dietary supplements cannot be billed as cures for these individuals, there is some research support that indicates many of the products in your store can add a layer of support for shoppers who are considering other ways to maintain their digestive health.
Chronic ≠ Hopeless
Before proceeding, it’s important to have some framework for understanding chronic digestive disorders. Individuals with Crohn’s disease and colitis experience inflammation in their gastrointestinal (GI) tract. In colitis, the inflammation is usually in the colon, which causes open sores, chronic pain and diarrhea. Crohn’s patients experience similar inflammation and sores, though it can affect patches anywhere in the GI tract (most often the small intestine).
Both illnesses have a commonality: the inflammation is the result of an abnormal immune system response. For reasons still unknown to the medical community, the immune system mistakes bacteria in the intestines for an invader and dispatches white blood cells there, which results in chronic inflammation and ulcerations (2).
Omegas. While no one is 100% sure of the exact causes of autoimmune diseases, some evidence suggests that dietary choices may play a role in certain individuals. For instance, some studies point to a link between a diet rich in omega-6 and the onset of some autoimmune diseases (like Crohn’s and colitis), while omega-3s may offer some benefits.
Individuals with Crohn’s and colitis may want to be especially careful not to consume a diet that is heavy in omega-6s and light in omega-3s. The reason why, says Fred Pescatore, M.D., M.Ph., C.C.N., author of The Hamptons Diet and Boost Your Health With Bacteria, is because omega-3s are anti-inflammatory and omega-6s are proinflammatory agents that upregulate the body’s prostaglandin pathways that cause inflammation “[This] is necessary to suppress in anyone, but especially in those with a disordered immune system,” he states.
Over time, this may lead to an inflammatory state in people with a predisposition for autoimmune diseases. In a study published earlier this year, researchers found that a diet rich in EPA and DHA (especially DHA) offered some protection against the development of ulcerative colitis in a trial of 25,639 people. The researchers state, “If the association is causal, then increasing the population’s intake of n-3 polyunsaturated fatty acids from oily fish may help prevent ulcerative colitis” (3). Several other studies have pointed to a similar conclusion in those with other autoimmune diseases like lupus and rheumatoid arthritis.
Two cytokines (interleukin 1 [IL-1] and leukotriene LTB) may be the reason for the link between omega-6s and autoimmune diseases in some people. According to Nena Dockery, scientific and regulatory affairs manager for National Enzyme Company, Forsyth, MO, immune cells make IL-1 to help regulate immune and inflammatory responses. Leukotriene LTB also helps sustain an inflammatory response. IL-1 and leukotriene LTB are derived from arachidonic acid, which form when omega-6 linoleic acid from vegetable oils breaks down to gamma-linolenic acid and then to arachidonic acid.
“Ideally, the production of arachidonic acid and hence these proinflammatory/ pro-immune cell-stimulating cytokines is modulated by omega-3 fatty acid,” states Dockery. “Unfortunately, the Western diet is composed of a disproportionate amount of omega-6 fatty acids resulting in an excess production of arachidonic acid and subsequently the pro-inflammatory cytokines. Not surprisingly, most autoimmune diseases are characterized by the presence of high levels of IL-1 and leukotriene LTB.”
Kaori Dadgostar, Ph.D., technical specialist for Jar row Formulas, Los Angeles, CA, adds to the discussion, observing, “Interestingly, in clinical studies, omega-3 fatty acid or fish oil supplementation significantly decreased the production of leukotriene B4 and overall rectal dialysates of leukotrienes in these patients.”
row Formulas, Los Angeles, CA, adds to the discussion, observing, “Interestingly, in clinical studies, omega-3 fatty acid or fish oil supplementation significantly decreased the production of leukotriene B4 and overall rectal dialysates of leukotrienes in these patients.”
Dadgostar further explains how omega-3 fatty acids help. They:
• reduce production of harmful prostaglandin E2 (PGE2) metabolite,
• suppress the formation of leukotriene B4, a pro-inflammatory molecule, and
• maintain or increase the production of beneficial prostaglandins.
“Even when Americans cut back on total fat consumed, their diets are still overloaded with omega-6 fatty acids and deficient in omega-3 fatty acids,” says Jo Kirst, technical expert for Schwabe North America, Inc., Green Bay, WI. “To get the ‘suggested’ amount of omega-3s, you’d have to eat at least two meals a week of oil-rich, cold water fish. And even that amount is not enough to get the clinical amounts necessary for maximum health benefits.” Thus, Kirst recommends taking a highquality omega-3 supplement like fish oil.
Of course, it is especially important to convey to shoppers that they should talk to his or her healthcare pr ovider before makes changes to one’s dietary regimen.
ovider before makes changes to one’s dietary regimen.
Enzymes. Because, as previously stated, Crohn’s and colitis are immune system disorders at their roots, some believe that systemic enzymes may benefit this group of people since enzymes help support a healthy immune system.
“A consistent use of systemic enzymes such as serrapeptase, pancreatin and nattokinase taken away from food by at least two hours supports the body in keeping the circulating immune complexes from attacking each other,” states Guy Devin, Ph.D., professional line broker and educator for Essential Formulas, Inc., Farmers Branch, TX. “They also help to rid the body of fibrin and fibrinogen, which are known to cover up these molecules and will slow the body’s ability to allow a proper immune response.”
Dockery agrees, adding further information about how animal, plant and microbial proteases selectively break up byproducts of inflammatory response. She states, “Many of them also are capable of inhibiting some of the pro-inflammatory cytokines involved in sustaining the inflammatory process. As a result, they may help relieve some of the symptoms associated with an autoimmune disorder.”
Dadgostar says some cli nical studies support the use of serrapeptase (and also bromelain) for reducing inflammation, though the research was not conducted on autoimmune diseases. In those recovering from inflammation caused by events like surgery and sports, enzymes helped speed recovery.
nical studies support the use of serrapeptase (and also bromelain) for reducing inflammation, though the research was not conducted on autoimmune diseases. In those recovering from inflammation caused by events like surgery and sports, enzymes helped speed recovery.
Another way enzymes support immune and digestive health is that they help the body reduce the amount of undigested food in the system, which could result in toxins. Says Dadgostar, “These toxins can interfere with proper intestinal function and can induce the formation of antigens and harmful deposits, which are responsible for the development of allergies and inflammatory aggregates. Since compromised gastrointestinal cell and immune functions as well as uncontrolled inflammation are the major causes of gastrointestinal autoimmune disease such as bowel disease, Crohn’s disease and ulcerative colitis, the aforementioned benefits of systemic enzymes may help prevent and/or treat these distressing diseases.”
Probiotics. Probiotics may be beneficial to those with autoimmune and inflammatory issues, says Devin. “The main benefit is to crowd out the bad bacteria thus providing good tight junctions within the gut and gastrointestinal track which will minimize any antigens from passing directly thru the mucosal lining which then can create the ill effect.”
When used in those with colitis, Scott Stobaugh, sales manager at Nutraceutix, Redmond, WA, explains that the probiotic delivery method is especially important. “The keys to quality probiotics are keeping the probiotic organisms alive through the manufacturing processes, alive on the retail shelf and alive during the transit past your stomach acids, so that they can reach your intestinal tract and provide optimal results,” he states. His company’s trademarked technology (LiveBac) is said to protect the probiotics from stomach acids and offer a controlled release so they are delivered throughout the intestinal tract. “This is especially crucial for people suffering with ulcerative colitis because the probiotic organisms need to reach the lower intestinal tract to provide the needed benefits to relieve their symptoms,” he explains.
Dadgostar adds that the probiotic Saccharomyces boulardii may be an especially good choice for those with an IBD because it can inhibit the production of cytokines and stimulate the activity of agents that protect the gut from inflammation.
The next section on irritable bowel syndrome offers some additional information about probiotics and intestinal health.
Strong nutritional base. Those with IBD may have difficulty absorbing enough nutrients, especially during a flairup of symptoms like diarrhea. So, be sure this clientele is aware of the value of a good multivitamin. Some clients may also have trouble absorbing B12 or fat-soluble vitamins, so be sure to have easily absorbable forms of those products in stock. 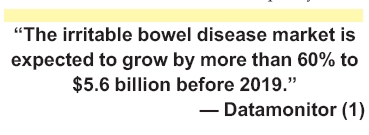
Address IBS Distress
Another chronic digestive condition affecting millions of Americans is irritable bowel syndrome (IBS). Unlike the previously mentioned IBDs, less-serious IBS doesn’t cause inflammation or permanent colon damage, though it can cause very uncomfortable symptoms like diarrhea, constipation, cramping and more. While the exact cause isn’t known, certain triggers of IBS may include certain foods, stress or illness (4).
Recently, probiotics have received much attention from the medical community as a way to support digestive health in those with IBS. Says Stobaugh, “Many GI physicians feel that IBS patients may have an overpopulation of certain ‘bad’ bacteria and if we can diminish these ‘bad’ bacteria and populate the intestines with ‘good’ bacteria from probiotics this will produce a beneficial effect. Probiotics produce bacteriocins, which kill foreign bacteria and prevent the bad bacteria from binding to the walls of your intestines.”
from binding to the walls of your intestines.”
Stobaugh adds that numerous randomized, placebo-controlled clinical trials involving people with IBS showed that “daily supplements of particular probiotic strains offer significant reductions in the symptoms of IBS, particularly for abdominal pain and bloating.”
Connie Falkenstein, R.D., M.S., MPH, director of marketing and education for UAS Laboratories, Eden Prairie, MN, speaks of a recent clinical trial conducted by University of North Dakota physicians and a Mayo Clinic researcher on a branded probiotic. This multispecies probiotic formulation (Probioplus DDS, from UAS Laboratories, Inc.) contained Lactobacillus acidophilus DDS-1, Bifidobacterium longum, Bifidobacterium lactis and Bifidobacterium bifidum with FOS. In the 25-person study, individuals showed much improvement in IBS symptoms including abdominal pain (84%), bloating (74%), belching (92%), flatulence (88%), diarrhea (91%) and constipation (87%) after two months, she explains.
“While the exact mechanism of action is not completely understood, one possible explanation is that an al ter - ation in the intest inal mi - crof lora and their metabolic end products is responsible for the symptoms of IBS,” Falkenstein explains. “Researchers used a double dose (20 billion CFU/g) in the first month and a normal dose in the second month. Improvement was classified as a minimum of 50% reduction in symptoms.”
And, Dadgostar cites other studies in which Lactobacillus plantarum 299v gave individuals “significant improvements” in symptoms like abdominal pain and bloating after four weeks (5) and in another study, patients showed a trend of normalized stools and stool frequency, while the control group showed very little change in symptoms (6).
The reason why probiotics may benefit those with IBS is that they “support the health and integrity of the intestinal mucosa, which can have far-reaching benefits,” says Dockery. For instance, probiotic bacteria that colonize in the intestines help improve mucosal integrity and barrier function, she says, while improving intestinal immune function, decreasing inflammation and possibly lowering the intestinal pH. “As a result, they effectively provide an overall healthier environment for optimal functioning of the gastrointestinal tract,” Dockery says.
Another way to support the intestinal lining may be with the amino acid, lglutamine. “It not only directly nourishes the mucosal lining of the intestine, but also helps repair it when it is damaged by hypersensitivity, physical stress, or an overreactive immune system. L-glutamine can stimulate the bowel to re-absorb water from the stool, reducing the number and frequency of bowel movements.”
Fiber may help the millions of American with IBS, since it helps reduce constipation in some people with IBS. Others find that fiber helps relieve diarrhea because it helps absorb excess water.
Peppermint oil is another traditional remedy for those experiencing stomach issues. According to Dadgostar, “Studies have shown that peppermint oil can relax the gastrointestinal tract sphincters and aid in the passage of gas,” which may benefit IBS patients. But, to reduce the risk of reflux, she suggests capsules be enteric coated.
And last, omega-3s may also bolster digestive wellness in those with IBS.
Heard About GERD?
A final condition that may affect a number of your shoppers is gastroesophageal reflux disease (GERD). This condition occurs when heartburn and acid reflux happen so often that the lower esophageal sphincter, the esophagus and other GI areas become damaged. According to Dadgostar, “The major contributor of this unpleasant condition is indigestion or overeating, either of which can leave a large amount of food sitting in the stomach.”
Digestive enzymes may help on this front because they help breakdown food. “A broad spectrum enzyme supplement that contains ample protease (protein digesting enzyme) may be essential for ensuring adequate gastric and overall digestion,” says Dockery, who notes that those with GERD may consider a gastric acid neutralizer if the esophagus has undergone significant damage. “If this is the case, the digestive functioning of gastric acid including its pivotal role in physical breakdown of food and activation of the protein digesting enzyme, pepsin, is compromised,” she says. D-limonene, found in citrus oils, is said to neutralize gastric acid and be suitable for those experiencing heartburn and GERD.
Stobaugh believes that probiotics are another good choice for people with chronic heartburn.
And, Pescatore recommends adding omega-3s (avoiding too much omega-6) and adding extra alkaline foods to the diet. WF
References
1. Datamonitor, “New Product Launches Drive Growth in Inflammatory Bowel Disease Markets,” press release distributed August 18, 2010.
2. Crohn’s and Colitis Foundation of America, www.ccfa.org/info/about/crohns, accessed Sept. 2, 2010.
3. S. John et al., “Dietary n-3 Polyunsaturated Fatty Acids and the Aetiology of Ulcerative Colitis: A UK Prospective Cohort Study,” Eur. J. Gastroente rol. Hepatol. 22 (5), 602–606 (2010).
rol. Hepatol. 22 (5), 602–606 (2010).
4. Mayo Clinic, “Irritable Bowel Syndrome,” www.mayoclinic.com/health/irritable-bowel-syndrome/ DS00106/DSECTION=causes, accessed Sept. 2, 2010.
5. P. Samart, J. Venkatraman and P. Ducrotte, “Evaluation of Lactobacillus plantarum 299v Efficacy in IBS: Results of a Randomized Placebocontrolled Trial in 200 Patients,” T2030- Poster Session: Prebiotics and Probiotics in the intestine: activities and function. Digestive Disease Week 2010, New Orleans, LA.
6. K. Niedzielin, H. Kordecki and B. Birkenfeld, “A Controlled, Double-Blind, Randomized Study on the Efficacy of Lactobacillus Plantarum 299v in Patients with Irritable Bowel Syndrome,” Eur. J. Gastroentrol. Hepatol. 13 (10), 1143–1147 (2001).
This editorial series is sponsored by Essential Formulas and Nutraceutix
![]()
Published in WholeFoods Magazine, October 2010.