With a fairly predictable regularity of once a decade or so, the general media likes to write articles questioning the safety of vitamin E supplements. It’s called “sensationalism press.” The idea is to get attention by going against common knowledge. It gains attention and sells papers. It’s fairly routine, but in August, I was really astonished to read two articles. One was entitled “An Overdose of Vitamin E Can Kill,” published on TheHealthSite.com (1).
The second alarming article from a supplements-friendly news service reported that bottles of a standard 400 IU vitamin E supplement had been seized by a European authority for allegedly being unsafe. The headline stated, “All Eyes on Supplement Sold with 77x Safe Vitamin E Levels” (2). This strength has been safely used since the early 1950s and even much higher strengths, including 1,000 IU soon after that. However, according to the aforementioned article, “The Luxembourg Ministry of Health was warning consumers not to buy a product containing 77 times the recommended safe daily dose of vitamin E.” The article went on to say, “The product contained a massive 400 IU of vitamin E—well over the 12 mg per day set for adults.
This ridiculous product “removal,” according to the article, involved an investigation of a global network of national food safety authorities managed by the Food and Agriculture Organization of the United Nations, the World Health Organization (WHO) and the International Food Safety Authorities Network (INFOSAN).
The Luxembourg Minister was reported as saying, “deficiencies in vitamin E were rare and excessive intakes of the vitamin were stored by the liver and had been associated with the onset of certain cancers” (emphasis added).
Relax—the safety of vitamin E is well established and reports of alleged association with causation of any disease have been debunked. Since there is once again a spate of safety questions, it is time to discuss the most recent research on the safety of vitamin E supplements. This month, I am calling upon vitamin E expert, Manfred Eggersdorfer, Ph.D.
Dr. Eggersdorfer is a professor of healthy aging at the University Medical Center Groningen (UMCG) in the Netherlands and the senior vice president of DSM Nutritional Products. He studied chemistry at the Technical University Munich and earned his Ph.D. in organic chemistry in the field of synthesis and characterization of unusual amino acids. He completed his post-doc at Stanford University, California, working with Carl Djerassi on the isolation and characterization of sterols from marine origin as potential contraceptives. He joined Roche in 1999 as head of research and development of vitamins and continued in this role after Roche was acquired by DSM in 2003. Dr. Eggersdorfer holds the chair for healthy aging at the UMCG and is responsible for nutrition science and advocacy at DSM Nutritional Products. His scientific work focuses on the role of essential nutrients for health, vitality and well-being, especially on the impact of inadequate intake and status of micronutrients on long term health and healthy aging. He is active as an advisory board member at the Johns Hopkins Bloomberg School of Public Health, the Strategy Board of the Institute of Food Science University Hamburg, and is an affiliate of various other organizations. He is the author of numerous publications in the fields of vitamins, innovation in nutritional ingredients and is a scientific reviewer for a variety of journals.
Passwater: Dr. Eggersdorfer, how did you become interested in vitamin E?
Eggersdorfer: I became interested in vitamin E because it is so important to health. Vitamin E is an essential micronutrient for growth and human health. Besides its recognized function as an important antioxidant in cell membranes in particular, it plays many roles in humans. Despite this essential role of vitamin E, many people all over the globe do not get adequate or optimal intake via the diet with consequences on long-term health.
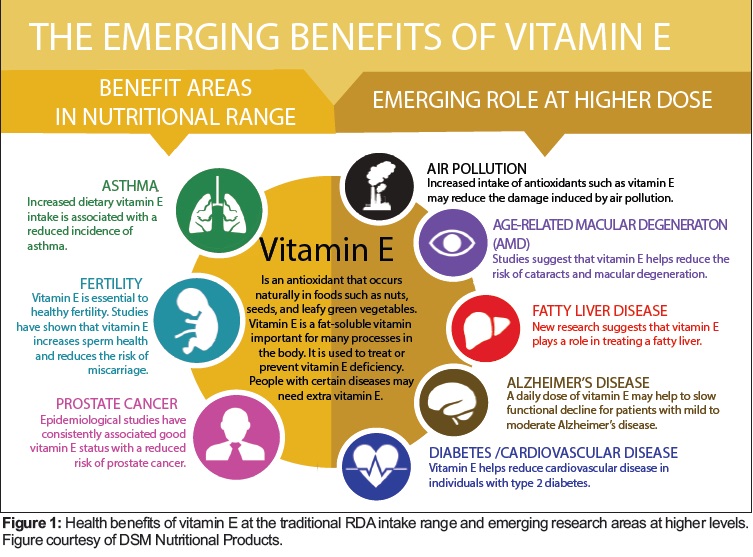
I advocate for the essential role of vitamin E for the general population in the Recommended Daily Allowance (RDA) range. I also believe all people should maintain healthy vitamin E levels in the body by consuming a balanced diet alone or in combination with a dietary supplement. I see new applications for higher vitamin E intakes for specific risk groups based on medical advice. Examples are people with age-related macular degeneration (AMD), those with poor glucose regulation and a certain polymorphism (HP2-2), people with fatty liver syndrome or those with mild cognitive impairment. These applications require higher doses of 400–2,000 mg/day to provide benefits.
Yet, surprisingly, some people argue that hard facts on benefits are limited. In my view, there are convincing data from many human studies addressing the aforementioned issues. However, we have seen a decline in vitamin E research in recent years. Considering the many roles vitamin E plays in the human body, I would like to see much more new research and science. This is the reason why I am calling for new projects to study the many functions of vitamin E, including investigating vitamin E gene interactions using biomarkers and new analytical tools and approaches to reevaluate the role and needs for health and wellness.
As researchers, we must stimulate new science on vitamin E. There is so much more to learn. We must advocate for an investment in new research and encourage young scientists to engage in new vitamin E research on nutrient-gene interactions. We must explore further how vitamin E can help maintain health. We must improve our understanding of the ideal daily intake levels for various populations. And then, we must let the public know the many health benefits of this essential vitamin.
Passwater: Before we get to the latest research on vitamin E safety, let’s put our readers at ease and review the official vitamin E guidelines prepared by U.S. Institute of Medicine (IOM). The IOM is part of the National Academy of Sciences (NAS) and has the responsibility by U.S. congressional charter to identify issues of medical care, research and education. It is composed of distinguished scholars. Within the IOM is the Food and Nutrition Board, which has expert panels on Dietary Antioxidants and Related Compounds and a subcommittee on Upper Reference Levels of Nutrients.
The summary of IOM’s 2000 report on Dietary Reference Intakes for Vitamin E states, “Human data fail to demonstrate consistently a causal association between excess alpha-tocopherol (vitamin E) intake in normal, apparently healthy individuals and any adverse health outcome” (3).
This sounds pretty safe to me. In non-scientific jargon, what is the plain English version of what the committee is telling us?
Eggersdorfer: Correct, vitamin E is safe in the range of daily usage and also at higher doses compared to the RDA, as has been demonstrated in numerous studies. Examples of studies with large population groups over several years are studies about AMD prevention with 400 mg/day (4), non-alcoholic fatty liver disease (NAFLD) with 800 mg/day (5) and studies in patients with Alzheimer’s disease (6). In these studies doses of 400-2000 mg/day per person were applied. In particular, these clinical studies in Alzheimer’s patients—which used a daily dose of 2,000 IU over two years with no reported safety concerns—may also provide a rationale to revisit the safety discussion.
However, if you have medical problems and take medications in combination with high dose vitamin E supplements, you should mention it to your doctor/pharmacist. They can then verify the compatibility of your medications with your vitamin E supplements, particularly with regard to blood coagulation status.
Passwater: The IOM determines safe limits called No-Observed-Effect Level (NOEL) and Lowest-Observed-Adverse-Effect Level (LOAEL). Do they also use the Observed Safe Levels (OSL) or Highest Observed Intakes (HOI), which to me are more meaningful because they are real clinical observations. What is the IOM guidance for vitamin E?
Eggersdorfer: Organizations like IOM assess the totality of the evidence and take any study into account those that seem to show adverse effects. To ensure the safe use of nutrients like vitamins and minerals, a so-called upper limit (UL) is defined. The UL defines the amount of a nutrient that can be taken safely over a long period. For vitamin E, the UL defined by IOM is 1,000 mg a day. In context, the IOM clearly states that a 400-IU product is safe. Agreed-upon procedures are in place for assessing the UL; one way is to start from the LOAEL in animal studies and apply factors to bridge from animals to humans.
In the case of vitamin E, IOM selected a LOAEL of 500 mg/kg body weight based on available animal studies. This is equivalent to 35 g/day (1.23 ounces/day) for a 70-kg (154-pound) person. A safety factor of 36 was applied, which resulted in an UL of 14 mg/kg body weight, equivalent to approximately 1,000 mg (1 g) per day for a 70-kg person (see p. 257 of IOM’s 2000 report on Daily Recommended Intake). This safety factor takes into account the uncertainty between the LOAEL and the NOAEL (no adverse effects level), chronic intake, the animal-to-human difference and inter-individual variation.
Passwater: Those guidelines are for the general public in free-living, unsupervised conditions. Haven’t higher dosages of vitamin E such as 2,000 or 5,000 IU or so been safely used in clinical studies? Do clinical studies have safety reviews?
Eggersdorfer: Correct, the Estimated Average Requirement (EAR) and RDA are defined based on intakes required to avoid deficiency diseases in populations. The UL guides the upper safety limit of regular intake. We know that in many cases, vitamins at higher doses may have additional beneficial effects. To study these benefits in humans, strict procedures are in place. Before any study can be initiated, it is evaluated by an Ethical Committee. During execution, the safety aspects of human studies are continuously monitored and evaluated by the study team and the Ethical Committee to ensure the safety and wellbeing of the participants.
Regarding vitamin E, numerous meta-analyses have been published during the last decade, aggregating the safety findings of dozens of randomized clinical trials. One example is Abner et al. (2011), who analyzed data from more than 246,000 subjects from 57 studies, receiving up to 5,500 IU/day vitamin E for 1–10 years (7). In accordance with the results of other meta-analyses on this topic, the conclusion was that supplementation with up to 5,500 IU vitamin E daily is safe.
Passwater: We’ve been focusing on the absence of risk with vitamin E supplements, but let’s look at the other side of the coin for a moment and discuss benefit. What is important in evaluating anything is the benefit-to-risk ratio. When I started my laboratory research with vitamin E in 1959, the U.S. Food and Drug Administration was still proclaiming that there was no need for vitamin E in humans. My research was with vitamin E as an antioxidant and free-radical scavenger. Are there functions of vitamin E in humans independent of vitamin E being an antioxidant such as in gene expression?
Eggersdorfer: In addition to its recognized function as an important antioxidant in cell membranes in particular, it has numerous other roles in humans such as interacting with more than 400 genes and is associated with risk reduction for many human health issues. The main actions of vitamin E can be summarized as:
• Vitamin E is a powerful antioxidant. Once oxidized, it can be regenerated by vitamin C.
• Vitamin E depletion and repletion affect gene expression in vitro in cells and in vivo in animals, which indicate broader effects.
• The incorporation of vitamin E into cellular membranes can alter the activity of membrane-associated proteins and change signal transduction pathways.
• Vitamin E contributes to the protection of cells from oxidative stress.
Dietary intake recommendations for vitamin E are established in many countries around the globe and refer to its important role in preserving the integrity of the cell membrane as a powerful chain-breaking antioxidant. In the United States, the RDA for vitamin E is 15 mg of alpha-tocopherol in adults for both men and women. This RDA is based on preventing deficiency, as measured by in vitro lysis of red blood cells.
So, the essentiality of vitamin E is well established and the intake needed to meet the RDAs can be achieved by a balanced diet. However, the RDA may not be optimal to maintain health of all cells in the body.
A vitamin E supplement of 200 mg/day in the elderly significantly reduced the risk of upper respiratory infections and showed a lower incidence of common cold (8). In addition, emerging data suggest that in diabetics carrying the haptoglobin genotype HP2-2, a daily intake of 400 mg of vitamin E significantly reduced a composite cardiovascular endpoint such as cardiovascular death, myocardial infarction or stroke (9).
In addition, several studies report an improvement in fatty liver disease (nonalcoholic steatohepatitis or NASH) by daily intakes of 400–800 mg vitamin E in both children and adults (5). A recent study found a reduction of functional decline in Alzheimer’s disease at an intake of 2,000 mg/day of vitamin E, confirming earlier findings (6).
Currently, available evidence is limited for a possible function of vitamin E in human health beyond its role as an essential micronutrient. However, encouraging data point to specific conditions and diseases at intakes that are not likely to be achieved through regular diet and that may be applicable for selected individuals and groups rather than for the general population. Figure 1 shows some of the emerging health benefits of vitamin E at intake levels above the RDA.
Passwater: The point that I am leading to is that we probably still don’t know all of the functions of vitamin E and that the RDA seems to be largely based on antioxidant function and the protection of polyunsaturated fats in the body. It is difficult to set an RDA for something that we don’t fully understand. The news article mentioned at the beginning reported the Luxembourg Minister as saying vitamin E deficiencies were rare (2). Who would benefit from vitamin E supplements?
Eggersdorfer: I read the article with the eye-catching title, “All Eyes on Supplement Sold with 77x Safe Vitamin E Levels” with interest (2). However, to me, it is apparent that the local authorities in this case did not consider the current intake recommendations and safety for vitamin E or mixed figures. The article does not educate readers about current vitamin E research.
In the article, it is also stated that vitamin E deficiencies are rare. This is true in the context that few people have very low vitamin E concentrations associated with red blood cell lysis. However, several publications recently reported that low vitamin E concentrations may be a major issue in places like Nepal, Bangladesh and Korea. Even if obvious vitamin E deficiency may be rare in industrialized countries, marginal intake of vitamin E is relatively common in many countries.
The “Nationale Verzehrsstudie” (translated as National Nutrition Study) for Germany found that 40% of the population does not get enough vitamin E compared to recommendations via the diet. National surveys for other places like the United Kingdom and the Netherlands report similar findings; in the United States, 90% of the population does not consume the recommended dietary intake of vitamin E (10). So, fortified foods or multivitamins may play an important role in closing the gap between intake via food and recommendations. Nationally representative data from the U.S. population find that about two-thirds of U.S. adults have plasma vitamin E concentrations below that measured in individuals consuming the RDA (11).
Coming back to the news article: A company imported and offered a dietary supplement with 400 IU of vitamin E (or 294 mg of vitamin E per capsule) in Luxembourg. Luxembourg has set a maximum level for vitamin E at 18 mg/day in food supplement, so this food supplement with 294 mg is 16 times above the limit of Luxembourg. It is also approximately one-quarter of the upper limit set by the IOM.
What is the lesson? The food supplement does not comply with the regulations in Luxembourg and actions should be taken in Luxembourg. However, the food supplement is in line with regulations that are in place for the safe intake of vitamin E in many other countries.
Coming back to the first part of your question: Vitamin E is recognized as a key essential lipophilic antioxidant in humans protecting lipoproteins as well as cellular and intracellular membranes from damage. The role of vitamin E in the protection and preservation of the functions of polyunsaturated fatty acids (PUFAs) is well established and structural analysis of the localization of vitamin E in membranes showed that it is positioned to protect the PUFAs of phospholipids.
So, vitamin E requirements are related to dietary PUFA intake. Evidence in humans indicates a minimal basal requirement of 4–5 mg/day of vitamin E when the diet is very low in PUFAs. The vitamin E requirement increases with a rise in PUFA consumption and with the degree of PUFA unsaturation in the diet. The vitamin E requirement related to dietary linoleic acid, which is the major dietary PUFA in humans around the world, was calculated to be 0.4–0.6 mg of vitamin E per gram of linoleic acid.
Animal studies show that for fatty acids with a higher degree of unsaturation, the vitamin E requirement increases almost linearly with the degree of unsaturation of PUFAs. Assuming a typical intake of dietary PUFA, a vitamin E requirement ranging from 12 to 20 mg of vitamin E /day can be calculated. Several guidelines recommend increasing PUFA intake as they have well-established health benefits. It is prudent to ensure an adequate vitamin E intake matches the increased PUFA intake, especially as vitamin E intake is already below recommendations in many populations worldwide.
Passwater: Now, let’s look at some recent studies. The media widely circulated concerns that high doses of vitamin E might reduce lifespan according to a couple of meta-analyses. What are the facts? Please explain what meta-analyses are. Do different methodological approaches result in varying conclusions? What did these meta-analyses actually show, and what didn’t they show?
Eggersdorfer: Meta-analyses are overall assessments across several comparable studies. They basically calculate a weighted average of the outcomes from selected studies. This weighted average can be heavily influenced by which studies are included and excluded. Several meta-analyses have been published about mortality associated with vitamin E supplementation. However, each meta-analysis included a somewhat different subset of the available studies and came to somewhat different conclusions.
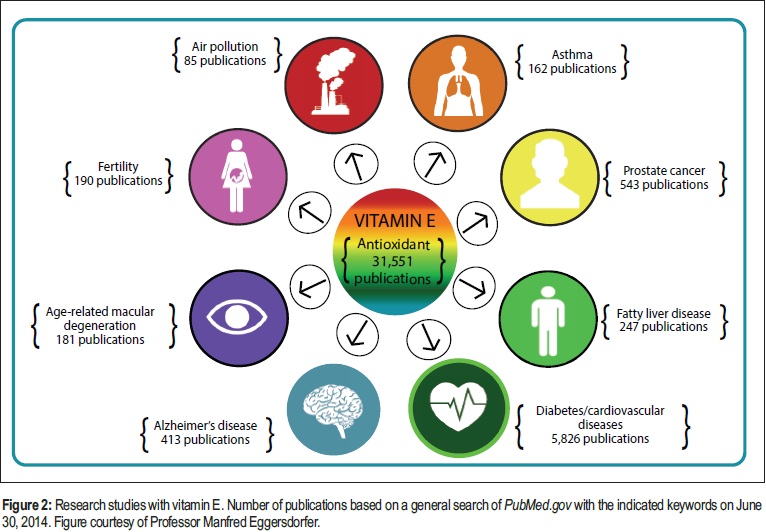
The total body of science is already extensive, but is still growing. Figure 2 illustrates the number of studies with vitamin E in various areas of research.
Passwater: What about concerns for increased cancer incidence? What does the recent body of science tell us?
Eggersdorfer: To address this issue and clarify related concerns, the authors of a 2014 publication in The American Journal of Clinical Nutrition examined whether supplementation with 400 IU of vitamin E every other day affects the risk of cancer events during post-trial follow-up of the Physicians’ Health Study II (12). After 10 years of treatment and four years of observational follow-up, in comparison with placebo, vitamin E supplementation had no effect on the incidence of total cancers, prostate cancer or on other site-specific cancers overall. Stratification by known cancer risk factors showed no significant interactions. In this large-scale randomized trial in men, vitamin E supplementation had no immediate or long-term effects on the risk of cancers.
Concerning women, in a more recent study published in September 2015 in Scientific Reports of Nature, investigators examined the associations between antioxidant vitamins, among them vitamin E, and the risk of cervical cancer in China (13). The case-control study involved 458 incident cases with invasive cervical cancer and 742 controls to assess the effects of diet or serum antioxidant vitamins. In general, higher serum levels of antioxidant vitamins were associated with a lower risk of cervical cancer after adjusting for potential confounders. Moreover, dietary intake of vitamin E was inversely associated with the risk of cervical cancer in this population. The less vitamin E in the diet, the higher the incidence of cervical cancer. More research is needed to elucidate the relationship between suboptimal vitamin E status and cancer.
Passwater: Heart disease is an area of research that I find especially interesting. I conducted an epidemiological study among 17,894 adults aged 50–90 in 1976 and groups at Harvard in 1993 suggesting that vitamin E intake in adequate amounts over an adequate period of time reduced the risk of heart disease (14). Eric Rimm, Sc.D.’s group at Harvard found in a study of 51,529 men that those who consumed 100 IU or more of vitamin E daily had a 37% reduction in heart disease (15). Meir Stampfer, M.D., Ph.D.’s group at Harvard studied 87,245 women and found that women who took 100 IU or more of vitamin E daily for two years or more had a 46% reduced risk of heart disease (16).
The operative words here are adequate dosage and time. Less of either was not found to be effective. This has led me to question any nutritional studies that do not use effective amounts over an effective timeframe. Even aspirin doesn’t affect a headache if an insufficient amount is taken. I am also very skeptical of studies that lump everyone together based merely on dosage and not time of taking that dosage. What about older individuals who after noticing a sharp decline in function decide that they must do something, so they start taking 1,000 IU, participate in a randomized clinical trial (RCT), and unfortunately pass away prematurely? They shouldn’t be lumped together with healthy people who have been taking the same dosage for decades before they entered the RCT.
These epidemiological studies add support to the thesis that vitamin E can help prevent heart disease, but epidemiological studies do not provide proof; they merely suggest study areas by randomized control trials. Not that all RCTs are accurate, as they, too, have several limitations, including the potential for masking beneficial effects in particular subgroups of the study population (17).
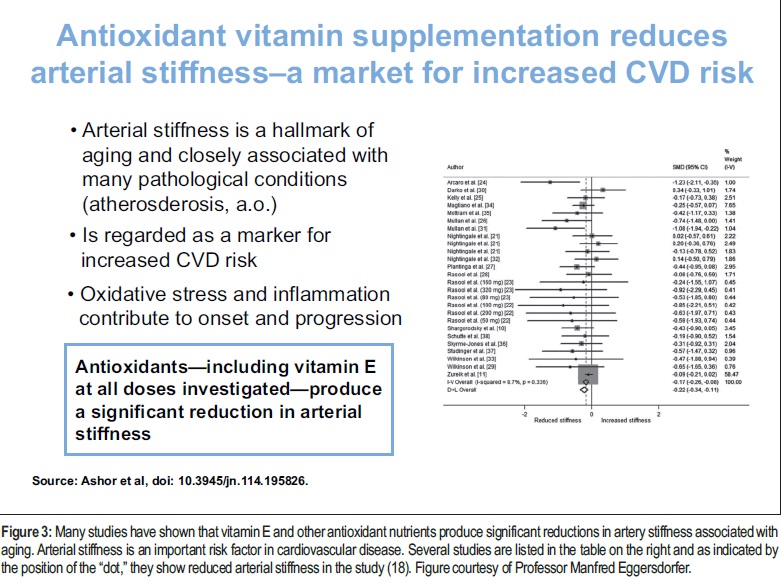
Antioxidant nutrients, including vitamin E, inactivate free radicals and also reduce inflammation. Both of these actions help protect the integrity of artery walls, primarily through reducing the replacement of elastin with collagen and with smooth muscle proliferation (17). Please note that this is protection of the arteries; it is prevention, not a cure. Once the elastin has been replaced by collagen it is difficult—but not impossible—to restore the arteries to their normal state. Researchers have begun to look into vitamin E actions on important biomarkers of cardiovascular disease such as artery stiffness. Arterial stiffness is closely associated with many diseases, including atherosclerosis, dyslipidemia, diabetes and chronic kidney disease (18). Arterial stiffness is regarded as a biomarker for increased cardiovascular disease risk and all-cause mortality (19).
Have studies shown that vitamin E reduces artery stiffness associated with aging?
Eggersdorfer: A meta-analysis conducted by John Mathers, Ph.D., and colleagues at the Human Nutrition Research Centre at Newcastle (UK) examined the effect of antioxidant vitamin supplementation on arterial stiffness in adults and concluded that there was a significant reduction in arterial stiffness with vitamin E and also with vitamin E combined with other antioxidant vitamins (20). Vitamin E was effective at all doses investigated. There were greater improvements observed with participants having lower levels of vitamin E in their blood at the beginning of the studies. Figure 3 illustrates these findings.
Passwater: That sub-group showed better results when the participants were more poorly nourished with antioxidant vitamins to start with may be masked in large RCTs and account for some of the failure for them to find positive results. Another sub-group of interest would be those who begin their vitamin E supplementation at earlier ages before irreversible damage occurs in the arteries such as elastin being replaced by collagen and smooth muscle proliferation.
Eggersdorfer: Another interesting observation reported in this study was that the response in arterial stiffness to supplementation differs for each particular vitamin, which suggests that each vitamin may have specific effects on artery walls, beyond the generic protective effects of antioxidant vitamins that you mentioned earlier.
Passwater: Indeed! Very interesting. The most recent findings that I am aware of establishing no harm from vitamin E supplements were published in 2014 and 2015. They include Jiang (2014), Curtis (2014), Paganini-Hill (2015) (21–24) and Lofreddo (2015). What do these studies teach us?
Eggersdorfer: We have recently seen several papers summarizing the findings of different studies on health outcomes. For example, Jiang and colleagues analyzed 19 RCTs with 80,283 subjects with a vitamin E intake ranging from 11 up to 5,000 IU/day for one to 10 years related to mortality (21). No impact on mortality (decrease/increase) is reported in this meta-analysis.
Curtis and colleagues published a meta-analysis based on 18 RCTs with 143,219 subjects and vitamin E supplementation in the range of 23-800 IU/day for 0.5 to 10 years (22). This analysis partly uses other RCTs compared to the analysis of Jiang and comes to the same conclusion that there is no change of mortality related to vitamin E supplementation. The same finding was reported in the Paganini-Hill paper this year (24).
The Lofreddo paper has a different approach looking at the relation of vitamin E supplementation and risk for myocardial infarct (23). The authors analyzed 16 RCTs with 74,192 subjects and vitamin E supplementation of 33–800 IU/day for 0.5 to 9.4 years. They report a 17% risk reduction for myocardial infarcts connected to vitamin supplementation.
These are just a few recent papers. Additional support for the safe use of vitamin E at higher doses comes from studies in people with mild to moderate Alzheimer’s or nonalcoholic steatohepatitis. In summary, these papers bring clarity to the ongoing controversy about the safe use of vitamin E at higher doses. I recommend to care for the adequate intake of vitamin E via a prudent diet and taking a supplement to fill the gap. Higher dose applications may have a benefit in people at risk and should be done under medical advice.
Passwater: That’s an important summary. Let’s further summarize. Dr. Eggersdorfer, as a leading vitamin E expert, what is your conclusion about the proven risks of harmful effects of sub-optimal vitamin E intake compared to the concern for speculative adverse effects of vitamin E supplements?
Eggersdorfer: You raise a very important question. We face vitamin E deficiency and insufficiency in many countries. Let me mention data from Keith West, Jr., Dr.PhH, MPH, of Johns Hopkins Bloomberg School of Public Health indicating vitamin E deficiency in Nepal and Bangladesh in the range of 30 to 60% is associated with a significantly higher risk for miscarriage. Another recent paper reported a deficient vitamin E status of 22% of South Koreans in Seoul (25). A deficiency range in these dimensions must be considered to be a public health issue and with an urgent need for governments and health authorities to act. Insufficient intake is an issue in the United States, where 90% of the population does not get enough vitamin E compared to recommendations, and the same is true in many other countries. The consequences of insufficient intake are more difficult to diagnose. Since the damage from moderate insufficient intake is insidious, its importance for long-term health is not clinically apparent. Mechanistic and epidemiological evidence suggests that the metabolic trade-off accelerates aging-associated malfunctions and diseases, such as cardiovascular disease, immune dysfunction and cognitive decline. A balanced diet, complemented with fortified foods and  supplements can markedly improve metabolism, health, vitality and support healthy aging.
supplements can markedly improve metabolism, health, vitality and support healthy aging.
Passwater: Thank you, Dr. Eggersdorfer. WF
Dr. Richard Passwater is the author of more than 45 books and 500 articles on nutrition. Dr. Passwater has been WholeFoods Magazine’s science editor and author of this column since 1984. More information is available on his Web site, www.drpasswater.com.
Published in WholeFoods Magazine, November 2015
References
1. www.thehealthsite.com/diseases-conditions/an-overdose-of-vitamin-e-can-kill-d915, accessed Sept. 24, 2015.
2. A-R Harrison-Rose “All Eyes on Supplement Sold with 77x Safe Vitamin E Levels,” Aug. 27, 2015, www.nutraingredients.com/Regulation-Policy/All-eyes-on-supplement-sold-with-77-x-safe-vitamin-E-levels, accessed Sept. 24, 2015.
3. Institute of Medicine, Food and Nutrition Board, “Dietary Reference Intake: Vitamin C, Vitamin E, Selenium, and Carotenoids,” National Academy Press, Washington, D.C., 2000.
4. E.Y. Chew, et al., “The Age-Related Eye Disease Study 2 (AREDS2): Study Design And Baseline Characteristics (AREDS2 report number 1),” Ophthalmol. 119 (11), 2282–2289 (2012). doi: 10.1016/j.ophtha.2012.05.027.
5. A.J. Sanyal, et al., “Pioglitazone, Vitamin E, Or Placebo For Nonalcoholic Steatohepatitis,” N. Engl. J. Med. 362 (18), 1675–1685 (2010). doi: 10.1056/NEJMoa0907929.
6. M.W. Dysken, et al., “Effect of Vitamin E and Memantine On Functional Decline In Alzheimer Disease: The TEAM-AD VA Cooperative Randomized Trial,” JAMA 311 (1), 33-44 (2014). doi: 10.1001/jama.2013.282834.
7. E.L. Abner, et al., “Vitamin E and All-Cause Mortality: A Meta-Analysis,” Curr. Aging Sci. 4 (2), 158–170 (2011).
8. H. Hemilä and E. Chalker, “Vitamin C for Preventing And Treating The Common Cold,” Cochrane Database Syst. Rev. 2013 Jan 31;1:CD000980. doi: 10.1002/14651858.CD000980.pub4.
9. U. Milman, et al., “Vitamin E Supplementation Reduces Cardiovascular Events In A Subgroup Of Middle-Aged Individuals With Both Type 2 Diabetes Mellitus And The Haptoglobin 2-2 Genotype: A Prospective Double-Blinded Clinical Trial,”Arterioscler. Thromb. Vasc. Biol. 28 (2), 341–347 (2008).
10. V.L. Fulgoni et al., “Foods, Fortificants, And Supplements: Where Do Americans Get Their Nutrients?” J. Nutr. 141 (10), 1847–1854 (2011). doi: 10.3945/jn.111.142257.
11. M.I. McBurney, et al., “Suboptimal Serum α-Tocopherol Concentrations Observed among Younger Adults and Those Depending Exclusively upon Food Sources, NHANES 2003-20061-3,” PLoS One 19;10(8):e0135510 (2015). doi: 10.1371/journal.pone.0135510.
12. J.M. Gaziano, et al., “Multivitamins in the prevention of cancer in men: the Physicians' Health Study II randomized controlled trial,” JAMA 308 (18), 1871–1880 (2012).
13. Guo L. et al., “Associations Between Antioxidant Vitamins And The Risk Of Invasive Cervical Cancer In Chinese Women: A Case-Control Study,” Sci. Rep. 5:13607 (2015). doi: 10.1038/srep13607.
14. R.A. Passwater, “Heart Disease and Vitamin E Study,” Prevention 28 (1), 63–71 (1976).
15. E.B. Rimm, et al., “Vitamin E Consumption And The Risk Of Coronary Heart Disease In Men,” N. Engl. J. Med. 328 (20), 1450–1456 (1993).
16. M.J. Stampfer, et al., “Vitamin E Consumption And The Risk Of Coronary Disease In Women,” N. Engl. J. Med. 328 (20), 1444–1449 (1993).
17. M.I. Correia and W.G. Haynes, “Arterial Compliance And Endothelial Function,” Curr. Diab. Rep. 7, 269–275 (2007).
18. N.A. Shirwany and M.H. Zou, “Arterial Stiffness: A Brief Review,” Acta Pharmacol. Sin. 31, 1267–1276 (2010).
19. S. Laurent and P. Boutouyrie, “Arterial Stiffness: A New Surrogate End Point For Cardiovascular Disease,” J. Nephrol. 20 (Suppl 12) S45–50 (2007).
20. A.A. Ashor, et al., “Antioxidant Vitamin Supplementation Reduces Arterial Stiffness In Adults: A Systematic Review And Meta-Analysis Of Randomized Controlled Trials,” J. Nutr. dodi: 10.3945/jn.114.195826.
21. S. Jiang, et al., “Meta-Analysis: Low-Dose Intake Of Vitamin E Combined With Other Vitamins Or Minerals May Decrease All-Cause Mortality,” J. Nutr. Sci. Vitaminol. (Tokyo). 60 (3), 194–205 (2014).
22. A.J. Curtis, et al., “Vitamin E Supplementation And Mortality In Healthy People: A Meta-Analysis Of Randomised Controlled Trials,” Cardiovasc. Drugs Ther. 28 (6), 563–573 (2014). doi: 10.1007/s10557-014-6560-7.
23. L. Loffredo, et al., “Supplementation with Vitamin E Alone Is Associated With Reduced Myocardial Infarction: A Meta-Analysis,” Nutr. Metab. Cardiovasc. Dis. 25 (4), 354–363 (2015). doi: 10.1016/j.numecd.2015.01.008.
24. A. Paganini-Hill, et al., “Antioxidant Vitamin Intake And Mortality: The Leisure World Cohort Study,” Am. J. Epidemiol. 181 (2), 120–126 (2015). doi: 10.1093/aje/kwu294.
25. Y-N. Kim and Y-O. Cho, “Vitamin E Status Of 20- To 59-Year-Old Adults Living In The Seoul Metropolitan Area of South Korea,” Nutr. Res. Pract. 9 (2), 192–198 (2015). doi: 10.4162/nrp.2015.9.2.










