The disease state known as diabetes mellitus involves dangerous blood sugar dysfunction, that much is certain. But this complex disease has many layers. There are questions regarding cause, risk, prevention, complications, means of support and potential solutions that must be addressed on an individual basis, but with an eye to the larger problem posed to society by diabetes and associated conditions.
In this feature, we tackle many of these issues through the lens of dietary supplements, including recent research, and a look at the marketing practices for products in this category. The market for supplements that target this area is relatively small at the moment, says Scott Steil, president of Nutra Bridge, Shoreview, MN. “However, my opinion is that it remains the biggest category of unmet market and customer need and will explode over the next few years,” he says. The alarming growth rates in both diabetes and obesity will be met with increases in the costs of treating these conditions, Steil believes. Therefore, increased attention to supplements that help maintain healthy blood sugar and insulin function will play a vital role in improving our society’s health.
Diabetes: The Science and Supplements
New insights into diabetes, as well as the interrelated set of conditions that can precede it (variously referred to as metabolic syndrome, syndrome X or prediabetes) are always pouring in. Likewise, the ways supplements can help turn the tide away from prediabetes and back toward health, or support those forced to deal with full-blown diabetes, are under constant analysis from researchers.
By way of a primer, Bilwa Bhanap, M.D., researcher with the Dr. Rath Research Institute, Santa Clara, CA, explains that metabolic syndrome is typically characterized by obesity, high blood pressure, high cholesterol and impaired glucose metabolism and insulin function. The sustained high blood sugar levels caused by these issues can lead to serious complications including atherosclerosis, stroke, kidney damage and failure, nerve damage, impaired wound healing, immune system issues, cataracts and a host of other issues, according to Bhanap. Most of these complications, she says, are due to blood vessel damage in the affected organs.
Though genetic factors are thought to play a role in the development of type 2 diabetes, it is more commonly linked with consuming high levels of artificial sugars, Bhanap says. Type 1’s causes are not well understood, though genetic and environmental factors such as viruses appear to play a role, according to Trisha Sugarek MacDonald, B.S., M.S., director of R&D and national educator for Bluebonnet Nutrition Corporation, Sugar Land, TX. Type 1 diabetes is most common in children and adolescents, though this autoimmune condition has also been diagnosed in adults, she adds.
Whereas type 2 diabetes is usually spoken of in terms of insulin resistance, in type 1 diabetes, the beta cells of the pancreas that produce insulin are destroyed by the body’s own immune cells. The result is a lack of insulin production, meaning glucose cannot be conveyed properly into the body’s cells. Troublingly, more children are getting diagnosed and treated for the complex risk factors that lead to type 2 diabetes, conditions which in the past had been mostly linked with aging.
terms of insulin resistance, in type 1 diabetes, the beta cells of the pancreas that produce insulin are destroyed by the body’s own immune cells. The result is a lack of insulin production, meaning glucose cannot be conveyed properly into the body’s cells. Troublingly, more children are getting diagnosed and treated for the complex risk factors that lead to type 2 diabetes, conditions which in the past had been mostly linked with aging.
Diet is important in preventing and improving metabolic syndrome and diabetes. Michael Smith, M.D., senior health scientist with Life Extension, Fort Lauderdale, FL and host of Healthy Talk on RadioMD.com, says that research shows a balanced diet composed of 15–20% of calories from protein, 25–35% from healthy fat and 45–55% from complex carbohydrates like leafy greens, grains and legumes can flatten out blood sugar spikes and improve insulin sensitivity. Jay Levy, director of sales at Wakunaga of America Co., Ltd., Mission Viejo, CA, says that along with diet and exercise, supplements should be a part of the plan for people with mild to moderate diabetes They can also help to reverse the risk factors that make up metabolic syndrome, including high blood sugar levels.
Though the fact that insulin resistance (rather than a lack of insulin) is most associated with type 2 diabetes might lead to the notion that supplements are only of help to those with type 2, Smith says this isn’t true. “In type 1, the patients inject insulin into their system. However, if they don’t follow the prescribed diets and exercise regimens, the injected insulin can begin to dysfunction in the same way that a person with type 2 experiences,” he says. Therefore, supplements that improve insulin sensitivity can help type 2 and type 1 diabetics alike.
Let’s examine those places where diabetes research and supplement science have overlapped most recently. To begin with, the connection between vitamin D status and insulin function is getting stronger. “One of the newer studies, which appeared in the April issue of the American Journal of Clinical Nutrition, found that correcting a vitamin D deficiency with supplements improves insulin sensitivity in overweight teens,” says Levy (1). Specifically, he adds, vitamin D improved fasting insulin levels and leptin-to-adiponectin ratios. This ratio is measured because unhealthy fat cells are thought to secrete more leptin and less of the protein adiponectin.
Another major vitamin has its place in this discussion, too. “It is important to note the similarity in the molecular structure of the sugar (glucose) molecule and the vitamin C molecule. This similarity is the key to understanding most of the cardiovascular complications in diabetes,” says Bhanap. She explains that the tiny pumps in blood vessel cells that are responsible for the transport of blood sugar in and out of cells are also tasked with bringing in vitamin C.
In diabetics, the excess of sugar in cells can therefore create a vitamin C deficiency resulting in fragile blood vessel walls. These are the areas, Bhanap says, most susceptible to the development of the atherosclerotic plaque that can lead to heart attacks, eye problems, kidney failure and other health problems.“Optimum daily intake of vitamin C helps to restore the balance between vitamin C and sugar metabolism inside the cells and prevent further complications,” she says.
Bitter melon (Momordica charantia) contains several compounds thought to help lower blood sugar, including insulin-like peptides, Levy says. He cites a study on bitter melon that confirms the mechanism through which it activates the AMPK enzyme (2). This enzyme, Levy explains, directly helps to lower blood sugar, and is the frequent target of anti-diabetes drugs. He adds that other research suggests bitter melon can improve insulin signaling and sensitivity.
 Though the arsenal of diabetes and blood sugar nutrients has been pretty well picked over, says Dallas Clouatre, Ph.D., consultant for R&D at Jarrow Formulas, Inc., Los Angeles, CA, the wild genotype of bitter melon is indeed an interesting option. He goes on to note that the similarities between the mechanisms of action of bitter melon and the diabetes drug metformin have been known for a few years, including the way they reduce excessive liver glucose output and reduce serum insulin.
Though the arsenal of diabetes and blood sugar nutrients has been pretty well picked over, says Dallas Clouatre, Ph.D., consultant for R&D at Jarrow Formulas, Inc., Los Angeles, CA, the wild genotype of bitter melon is indeed an interesting option. He goes on to note that the similarities between the mechanisms of action of bitter melon and the diabetes drug metformin have been known for a few years, including the way they reduce excessive liver glucose output and reduce serum insulin.
Now, in a more recent study on diabetic animals, wild bitter melon has been shown to rival metformin in regulating blood glucose, and to be superior to two commercial extracts of cultivated bitter melon in nitric oxide generation (key for maintaining healthy blood pressure) and inhibition of the angiotensin-converting enzyme (ACE) (3). “These facts suggest that wild bitter melon, especially if properly extracted and preserved, may perform some of the other functions of metformin, as well, such as encouraging weight loss,” Clouatre says. To cap off the bitter melon discussion, he adds that it can counterbalance the impact of fructose on the liver. Overconsumption of the simple sugar fructose can cause liver dysfunction by spurring the synthesis of fat and interfering with the liver’s response to insulin signals, he says.
In the majority of cases of diabetes and metabolic syndrome, gluconeogenesis develops, meaning the liver continues to release glucose into the bloodstream, even though levels of insulin and blood sugar would be adequate to inhibit this action in a healthy person. In addition to bitter melon, Clouatre says green coffee bean extracts can help to regulate the liver, in part by reducing liver gluconeogenesis. Restoring proper liver function is crucial to improving non-alcoholic fatty liver disease (NAFLD). We will discuss NAFLD more later, but for now, Clouatre notes that improving this condition may also benefit many aspects of diabetes, including blood sugar.
Since improving upon insulin dysfunction in daily life is a primary goal in dealing with diabetes, any ingredient found to help with that task will be of special interest. By blocking both the alpha amylase and alpha glucosidase enzymes, and thereby helping regulate insulin and glucose, a seaweed extract ingredient (InSea2 from Nutra Bridge) fits the mold. Steil explains that by blocking these two enzymes, the glycemic impact of both starch and table sugar are lessened. The ingredient, therefore, offers more complete control of blood sugar than other ingredients that block only carbohydrates.
After pointing out the difficulty of totally avoiding starch and complex carbohydrates in the diet, Steil explains that supplementing with this ingredient can help reduce the quick spikes in blood glucose and insulin associated with many foods. The ingredient has been found to reduce glucose levels by 48%, peak insulin levels by 22% and total insulin levels by 12%, and to increase insulin sensitivity by 8% when compared with placebo, according to Steil. In essence, this equates to helping convert starch-rich meals from high to low on the glycemic index, an important factor for diabetics and prediabetics.
Salacia (Salacia oblonga), according to Levy, is an Ayurvedic herb also thought to help prevent blood sugar spikes via a carbohydrate enzyme-blocking mechanism. Preliminary research performed on rats found that salacia lowered blood glucose by up to 45% while boosting HDL, or good cholesterol (4). Another option that slows the rate of both the digestion and uptake of carbohydrates and sugars is white bean extract, according to Clouatre. It is perhaps best known as a carbohydrate blocker meant to reduce blood glucose levels.
Dietary fiber can play a major role in this struggle of  diabetes sufferers to turn their glycemic luck around. Michael Arlen, president of NEWtritious, LLC, Los Angeles, CA, describes research he saw presented at a conference by a team of scientists from Japan. “They reported that there was a remarkable difference in the glycemic index based on the order in which foods were eaten!” he says. During the study, two groups ate the same meal, but one group was instructed to eat the green vegetables first, and other to eat the rice and meat first. There was a significantly lower glycemic impact in those that started off with the veggies. Though Arlen thinks this warrants further study, he feels the public should be made aware that they might help flatten out glycemic spikes, which can cause inflammation and degenerative disease, through such simple actions.
diabetes sufferers to turn their glycemic luck around. Michael Arlen, president of NEWtritious, LLC, Los Angeles, CA, describes research he saw presented at a conference by a team of scientists from Japan. “They reported that there was a remarkable difference in the glycemic index based on the order in which foods were eaten!” he says. During the study, two groups ate the same meal, but one group was instructed to eat the green vegetables first, and other to eat the rice and meat first. There was a significantly lower glycemic impact in those that started off with the veggies. Though Arlen thinks this warrants further study, he feels the public should be made aware that they might help flatten out glycemic spikes, which can cause inflammation and degenerative disease, through such simple actions.
Arlen also points to research on the effect fiber has on satiety, weight reduction and the eventual improvement of biomarkers for diabetes. “Certain soluble fibers have been shown to lower triglycerides in the blood,” he says. In addition to a slew of proprietary ingredients with impressive research backing, Arlen tabs konjac root, which contains a fibrous substance called glucomannan, for its ability to support diabetes.
“The effectiveness of any fiber on reducing appetite, blood sugar and cholesterol is based directly on the amount of water the fiber is able to absorb and the degree of thickness or viscosity the fiber imparts when in the stomach and intestine,” says Michael T. Murray, N.D., director of product development and education at Natural Factors Nutritional Products, Inc., Everett, WA. The solubility and viscosity of oat bran, he says for example, allows it to support cholesterol and control blood sugar more effectively than wheat bran.
Research has shown one proprietary fiber matrix (PGX from Natural Factors) to exhibit these benefits in a powerful way. The specific areas it supports, according to Murray, range from helping to stabilize blood sugar in the overweight and obese, to reducing appetite, reducing after-meal glucose levels, lowering blood cholesterol and triglycerides, increasing insulin sensitivity and more.
As Murray explains it, the reason weight control is so central to improving one’s chances against diabetes is that fat cells, or adipocytes, secrete a number of molecules that can have negative effects. Adipocytes around the abdomen in particular, when they become full of fat, release resistin, leptin, tumor necrosis factor, free fatty acids and cortisol, which combine to dampen the effect of insulin, impair insulin release by beta cells in the pancreas, impair glucose metabolism in skeletal muscle and promote liver gluconeogenesis. In fact, according to Murray, all the hormones newly discovered to be secreted by adipocytes have some experts considering adipose tissue as an element of the endocrine system (which includes the thyroid, adrenal and pituitary glands).
 Murray adds that as the size and number of adipocytes increases, the release of compounds that promote insulin function is reduced, including adiponectin. “Adiponectin is not only associated with improved insulin sensitivity, but it also has anti-inflammatory activity, lowers triglycerides, and blocks the development of atherosclerosis,” he says. The total effect of these actions on the part of fat cells is a severely stressed blood glucose control system, and an environment conducive to atherosclerosis.
Murray adds that as the size and number of adipocytes increases, the release of compounds that promote insulin function is reduced, including adiponectin. “Adiponectin is not only associated with improved insulin sensitivity, but it also has anti-inflammatory activity, lowers triglycerides, and blocks the development of atherosclerosis,” he says. The total effect of these actions on the part of fat cells is a severely stressed blood glucose control system, and an environment conducive to atherosclerosis.
Early on, Murray says the metabolic stress created by unhealthy adipoctyes may not affect blood glucose levels, as the pancreas simply responds with more insulin output. As the stressors increase and insulin resistance grows, the pancreas eventually cannot compensate. At this point, blood glucose can elevate, and as the condition progresses to full-blown diabetes, the insulin output from the pancreas can begin to decrease. Fortunately, Murray explains, the pancreas can recover if one works to improve insulin sensitivity and to achieve ideal body weight. Moving forward, he believes blood levels of adiponectin and other hormones secreted by fat cells may become meaningful risk factors for type 2 diabetes.
Echoing Murray on the relevance of toxic belly fat to diabetes, Don VerHulst, M.D., chief science officer of InBalance Health, Wayland, MI, says, “In my opinion, the best recent science on diabetes was done at Johns Hopkins, and correlated waist measurement with risk of type 2 diabetes.” Reviewing data from upwards of 27,000 men over a 13-year period, researchers found almost exponentially greater risk of the disease with larger waistlines. Compared with the group with the smallest waist circumference, those who had 40- to 62-inch waists were 12 times more likely to develop diabetes (5). “This study proved that your waistline is your life line,” says VerHulst.
Toxic belly fat can indeed become responsible for a vicious cycle of insulin resistance leading to higher blood sugar, which can in turn create more belly fat. But, VerHulst thinks the cycle can be broken by addressing the root cause. He states, “The future in successful treatment and prevention of type 2 diabetes, I believe, should and will focus on correcting insulin resistance by removing excess belly fat.”
Though supplements can help in this area, VerHulst cites the importance of regular exercise in maintaining weight. “Even the Centers for Disease Control and Prevention tells us that losing only 5 to 7% of your body weight and exercising 30 minutes five times a week can prevent the progression of a prediabetic state to full-blown diabetes. This progression will occur in about 30% of prediabetics within three to five years if nothing is done to stop it,” he says.
The actions of healthy fat cells, as just discussed, can help to control inflammation rather than cause it. This is key in the fight against diabetes because of the role of inflammation in general. A primary reason that sustained high blood sugar can be damaging is that it leads to oxidative stress and inflammation. Educator and author Andreas M. Papas, M.Sc., Ph.D., on behalf of A.C. Grace Company, Big Sandy, TX, addresses the inflammation issue. Papas was assisted in his responses by Allison Corkey and Klearchos Papas, Ph.D.
Emerging experimental evidence has improved 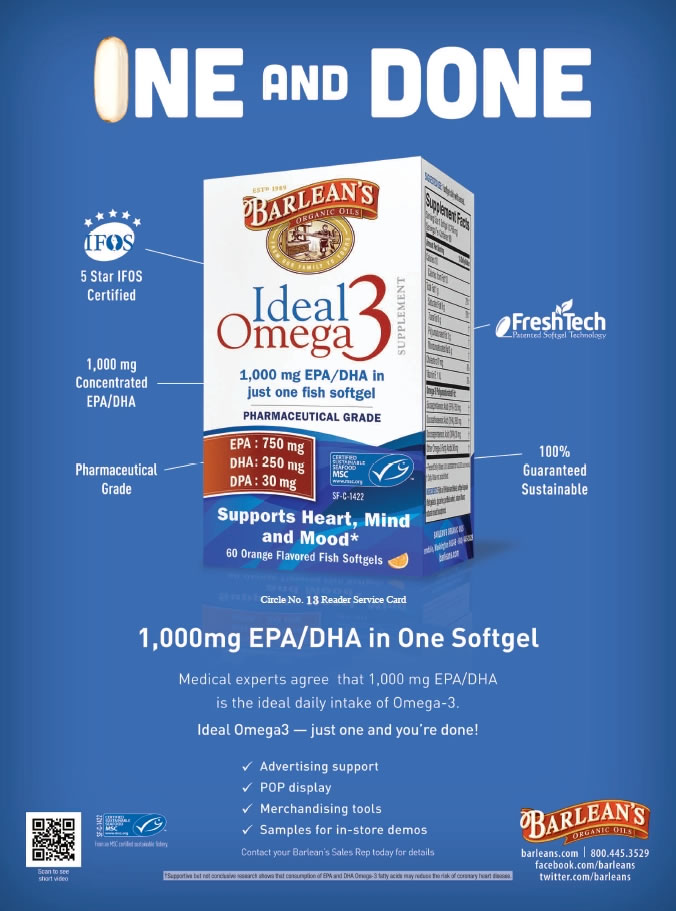 our understanding of the way oxidative stress underlies diabetes and its complications, according to Papas. In diabetics, excessive free radicals are formed by glucose oxidation, nonenzymatic glycation of proteins, and the oxidative degradation of those glycated proteins, he explains, stating, “Abnormally high levels of free radicals and the resulting decline of antioxidant defense mechanisms can lead to damage of cellular organelles and enzymes, increased lipid peroxidation and the development of insulin resistance that is associated with type 2 diabetes.” Tissues that are highly dependent on oxygen for energy production, like cardiac muscle, the nervous system, and insulin-producing pancreas cells, are prime areas for these defective oxidative processes, according to Papas.
our understanding of the way oxidative stress underlies diabetes and its complications, according to Papas. In diabetics, excessive free radicals are formed by glucose oxidation, nonenzymatic glycation of proteins, and the oxidative degradation of those glycated proteins, he explains, stating, “Abnormally high levels of free radicals and the resulting decline of antioxidant defense mechanisms can lead to damage of cellular organelles and enzymes, increased lipid peroxidation and the development of insulin resistance that is associated with type 2 diabetes.” Tissues that are highly dependent on oxygen for energy production, like cardiac muscle, the nervous system, and insulin-producing pancreas cells, are prime areas for these defective oxidative processes, according to Papas.
Oxidative stress, especially through nitrogen radicals, contributes to inflammation, which evidence links to the development of diabetes. Papas says that pro-inflammatory cytokines including C-reactive protein, tumor necrosis factor (TNF)-alpha and interleukin (IL)-6 are found in increased levels in diabetics. These factors can lead to the major complications seen in some diabetics. “Strategies that reduce oxidative stress and inflammation provide a powerful tool in the prevention and management of diabetes, especially when combined with lifestyle modification,” Papas says.
One avenue toward reducing inflammation is presented by vitamin E. The antioxidant capacity of vitamin E, which is actually a class of eight compounds, four called tocopherols and four called tocotrienols, has been brought to light by research, according to Papas. Food sources can contain all eight, and are typically rich in gamma tocopherol. In research circles, vitamin E had been synonymous in the past with only alpha tocopherol, which has led to its efficacy for various health purposes being questioned.
But gamma tocopherol, Papas says, along with its metabolite, is an effective quencher of nitrogen radicals. Tocotrienols, particularly alpha tocotrieonol, inhibit phospholipase A2, which releases fatty acids. Gamma tocotrienol, in particular, suppresses production of HMG-CoA, which is involved in LDL cholesterol production and is targeted by statin drugs, according to Papas. The general anti-inflammatory actions of the entire vitamin E class of compounds, he emphasizes, are especially applicable to diabetes.
Vice president of Edison, NJ-based Carotech, Inc., W.H. Leong, says that studies suggest the polyunsaturated nature of tocotrienols contribute to their unique potency. In addition to cholesterol support, anti-inflammation and antioxidant function, tocotrienols have been found to benefit the related areas of blood pressure support, blood glucose maintenance and insulin sensitivity, according to Leong. A palm oil-derived mixed tocotrienol/tocopherol complex (Tocomin from Carotech) has been shown to improve insulin sensitivity and glucose utilization in diabetic mice (6).
This vitamin E complex has also been studied in the context of liver function, specifically NAFLD. Leong describes NAFLD as a main risk factor for type 2 diabetes, since the liver helps to regulate glucose levels along with other functions. Where NAFLD is found, so too are obesity, insulin resistance and hyperlipidemia.
“A formerly rare condition, the rapid emergence of NAFLD has been linked to skyrocketing rates of metabolic syndrome and ‘diabesity’—the term many experts use for co-occurring diabetes and obesity,” Leong says. A version of the previously described proprietary vitamin E complex was used in an interventional, double-blind, placebo-controlled human clinical trial on 64 subjects over the period of a year. 50% of the subjects that received the vitamin E complex saw complete remission of NAFLD, compared with 23% for the placebo group (7). Leong calls this the first study to demonstrate the efficacy of tocotrienol for NAFLD.
 The list of nutrients that can fill the antioxidant role and perform other functions in support of diabetes continues with omega-3 fatty acids. “Because of their significance as structural components of critical organs, their role in cardiovascular health and their anti-inflammatory effects, omega-3 fatty acids can play a significant role in the management of diabetes,” says Papas. The omega-3 DHA, he explains, is a primary component of the brain, retina, skin, sperm and testicles. Omega-3s in general, he adds, have been shown to improve blood lipid profiles and reduce levels of inflammatory mediators.
The list of nutrients that can fill the antioxidant role and perform other functions in support of diabetes continues with omega-3 fatty acids. “Because of their significance as structural components of critical organs, their role in cardiovascular health and their anti-inflammatory effects, omega-3 fatty acids can play a significant role in the management of diabetes,” says Papas. The omega-3 DHA, he explains, is a primary component of the brain, retina, skin, sperm and testicles. Omega-3s in general, he adds, have been shown to improve blood lipid profiles and reduce levels of inflammatory mediators.
Coenzyme Q10 (CoQ10) is a crucial part of the electron transport chain involved in respiration, and has a high concentration in the heart, Papas says. This important antioxidant is also key for mitochondrial energy production. Inefficient respiratory chain function is one way free radicals get produced, he says, adding, “Diabetes is associated with low blood levels of CoQ10, and diabetics are at higher risk of mitochondrial and other diseases associated with mitochondrial function.”
The carotenoids lutein and zeaxanthin are both components of the retina and are important for diabetics, Papas says, because retinopathy is often a problem. Other carotenoids like beta-carotene, lycopene and astaxanthin exhibit antioxidant properties and may also be helpful. Alpha-lipoic acid is an essential cofactor for mitochondrial enzymes, Papas says, and may help with glycemic control and neuropathy. Clouatre says that the newer, stabilized form called R-alpha lipoic acid is likely the supplement of choice.
Adding in another antioxidant, Levy says, “Several studies suggest aged garlic extract inhibits the formation of advanced glycation end products that can contribute to diabetic complications.” In a related function, aged garlic extract can also reduce the formation of free radicals, according to Levy.
A proprietary extract of the maitake mushroom (Maitake SX-Fraction from Mushroom Wisdom) has shown blood sugar support benefits, according to Donna Noonan, senior vice president of Mushroom Wisdom, Inc., East Rutherford, NJ. “Studies at Georgetown University and New York Medical College confirm that SX-Fraction possesses a potent ability to enhance insulin sensitivity,” she says. One study using five volunteers with type 2 diabetes showed improved blood glucose levels in two to four weeks with the extract. Noonan says that while this trial was small, the balance of maitake extract research over the last 25 years shows a link with peripheral insulin sensitization and glycemic control.
Papas also lists cinnamon, as well as the minerals magnesium, chromium and vanadium for diabetes support. Chromium, Levy says, has a well-earned reputation for aiding blood sugar control. An essential trace mineral, it aids in processing carbohydrates and fats, and helps the body properly respond to insulin. A randomized, double-blind, placebo-controlled study found a proprietary chromium complex (Zychrome from InterHealth Nutraceuticals) to significantly decrease insulin resistance by 29.9% compared to baseline (8). Paul Dijkstra, CEO of InterHealth Nutraceuticals, Benicia, CA, says, “It is important to work with a doctor to take actions to reduce insulin resistance and lower fasting insulin and glucose levels. People may have insulin resistance for several years without noticing anything.”
Combining chromium picolinate and niacin, Levy notes, enhances the mineral’s absorption. In addition to this function, niacin, one of the B vitamins, also helps convert carbohydrates to energy, and research suggests it is involved in insulin metabolism and blood sugar regulation, according to Levy.
|
Diabetes Support Offerings The products and A.C. Grace Company: Unique E Mixed Tocopherols Concentrate, Unique Omega E+, Unique Derma+. |
|
“Another important aspect of supporting healthy blood sugar levels is supplying, at the cellular level, key nutrients to feed the pancreas and support healthy insulin production,” says VerHulst. According to Clouatre, one herb stands out in this context. “Gymnema sylvestre is the best known and best researched of the herbs that increase insulin release,” he says. However, he explains that while increasing insulin release can improve blood sugar levels, for those who are already dealing with insulin resistance, this may not be the best angle of approach. “Most prediabetics do not need to release more insulin, but rather to respond more appropriately to small amounts of insulin,” says Clouatre.
In addition to wild bitter melon and green coffee bean extract, Clouatre says, “In recent years, a great deal of attention has been directed toward cinnamon extracts as insulin sensitizers.” It may work by preventing and reversing impaired insulin signaling in skeleton muscle, and by promoting the expression of peroxisome proliferator-activated receptors in adipose tissue, he says.
Examining the synergistic effects of using nutrients in certain combinations is the focus of Bhanap’s company. “For example, arginine and other amino acids act synergistically to increase insulin secretion and insulin sensitivity,” she says, adding that the B vitamin thiamine and grape seed extract are other examples of diabetes-support nutrients that can be added to formulas.
Bhanap says a study compared the effects of a combination of nutrients to the drug metformin on several blood parameters of young, immature mice receiving a high fructose diet. The nutrient combination was found to reduce high blood pressure, high cholesterol and serum fructosamine (9). This last measure is often used to monitor blood glucose levels over periods of one to three weeks, according to Bhanap. To summarize, she states, “The synergy of essential vitamins, minerals and bioactive plant substances supports healthy glucose and carbohydrate metabolism.”
Factors, overlooked. As progress is made in diabetes research, new risk factors are sometimes revealed, or a new emphasis can be placed on a previously obscure cause. Some of these cases have already been discussed in our review of the latest science. Here are a few more potentially overlooked risk factors and support options tagged by our experts.
“Statin drugs are some of the most widely prescribed drugs in the world to help maintain healthy cholesterol; however, their role in raising the risk of diabetes has been observed and studied only in recent years,” says Sugarek MacDonald. Statins reduce cholesterol by blocking HMG-CoA, but they are also suspected of reducing levels of CoQ10 by this same pathway. Research has shown that supplementing with CoQ10 while taking statin drugs may help reduce the risk of diabetes by preventing statins from reducing levels of the compound GLUT4. “Altered levels of GLUT4, a compound that helps to control blood sugar levels, may contribute to insulin resistance and the onset of type 2 diabetes,” Sugarek MacDonald says, adding that further study of this effect is warranted in animals and humans.
Magnesium has been listed as useful for diabetes, but Clouatre points out it may be more necessary than many realize. “We as a nation are not fond of green leafy vegetables or of whole grains and, as a result, a majority of all Americans consume inadequate magnesium,” he says. A recent trial of overweight subjects supports the idea that magnesium plays a beneficial role in insulin regulation (10).
An important consideration, according to Murray, is an individual’s level of exposure to Persistent Organic Pollutants (POPs). These include such chemicals as polychlorinated dibenzo-p-dioxins (PCDDs), polychlorinated dibenzofurans (PCDFs), hexachlorobenzene (HCB), organophosphates, DDE and Bisphenyl A. As a group, they have been linked to the development of type 2 diabetes. Murray says, “Those with levels of organochlorine pesticides in the top quartile have a five times greater risk for metabolic syndrome.”
Levy reminds us that many of the plant-based options for supporting healthy cholesterol levels also impact diabetes positively. Phytosterols tied to reductions in LDL cholesterol also were of benefit to those with metabolic syndrome in a recent study (11).
The overarching impact of stress and depression on diabetes risk is worth discussing at length. In his book 30 Quick Tips for Better Health, VerHulst highlights the importance of stress management for controlling blood sugar. According to Clouatre, uncontrolled stress activates the hormone cortisol in a way that promotes glucose release from the liver and lean tissues, in order to prepare for “fight or flight” reactions that are usually not necessary.
“While the role of genetics, weight, diet and exercise are universally accepted, the role of stress, emotional health and depression are receiving attention both as contributing factors and also as complications of diabetes,” Papas says. Studies have tied high cortisol levels to heightened risk of both cardiovascular disease and diabetes. Normally, the “fight or flight” response subsides when the threat is removed, but if stress is chronic, blood sugar and insulin remain abnormally high, Levy explains.
Emotional disorders can also be considered a compounding factor for diabetics. Papas cites a study involving 42,000 people diagnosed with both untreated depression and diabetes. A 1.5- fold higher risk of death was found in those with both conditions (12).
An important consideration is the fact that responding positively to stress improves one’s ability to control its negative aspects. To illustrate, Clouatre cites a Swedish study that found work stress and shift work may contribute to type 2 diabetes risk in women, but in men, risk was decreased by high work demands, high strain and an active job (13). Thus, the context of stress helps determine whether it might contribute to diabetes.
The basic link is clear, as Papas emphasizes that stress, both physical and emotional, is linked with increased oxidative stress and inflammation. “It is also important to note that nutrients and natural compounds such as minerals, vitamins, antioxidants, omega-3 fatty acids and others have been shown to support emotional health and help reduce the risk of depression,” he says.
Levy suggests practices including meditation, yoga and exercise to relieve chronic stress and possibly mild depression. He says supplements that can help with stress include l-theanine and rhodiola, while SAMe, 5-HTP and St. John’s wort have been tied to depression support.
Navigating the Market
Perhaps more so than any other large segment of the supplement market, the diabetes support space is linked with a specific disease state. Those who participate in this space must therefore tread more lightly when it comes to terminology and health claims, and selling these products comes with a similar set of concerns. Federal Trade Commission (FTC) and U.S. Food and Drug Administration (FDA) oversight ensure that explicit links between supplements and the disease are kept in check.
VerHulst explains that his company avoids making problematic claims by saying its product supports the body’s ability to get and stay healthy. Indeed, as things stand now, natural diabetes-support products typically use general descriptions to imply management of healthy blood sugar levels, Leong exlplains. “Words such as ‘diabetes’ or ‘insulin resistance’ are highly sensitive and attract the attention of the authorities as they imply treatment of disease conditions,” he says.
Manufacturers that utilize ingredients in this category have to look at the science to see exactly how they can position products for consumers, including what structure/function claims can be used in marketing materials and on the product label, according to Dijkstra. “Ingredients that have been clinically shown to benefit blood sugar and/or insulin levels can take advantage of a ‘blood sugar management’ product positioning,” he says. Consumers may be looking for something more specific, Dijkstra adds, but manufacturers need to abide by regulations like the Dietary Supplement Health and Education Act (DSHEA), which sometimes makes it difficult to communicate clinically studied benefits to consumers.
Since the enactment of DSHEA, Noonan says, it has been clear what may be said and what may not be said about supplements, diabetes-support products included. “DSHEA says that dietary supplements may support the structure and function of an organ or system of the human body. Supplements that fall into this particular category may support blood sugar levels,” she says.
“Clearly, disease claims must be avoided. However, supplements can play a vital role in helping consumers address key blood sugar health concerns,” says Steil. His company has elected to work with terms that avoid disease claims while highlighting key benefits such as “reduced post-meal blood glucose and insulin levels” and “lower glycemic index.” Steil feels metabolic syndrome is also an area that supplement companies can target, as it is not considered a disease state.
Steil says such terms and phrases resonate with consumers, as certain groups may focus in on maintaining healthy blood glucose levels, while others may be looking for help with the glycemic index of the food they eat. Most consumers, he adds, will focus on healthy insulin levels, since this represents the core concern for diabetics and prediabetics.
“Structure and function claims remain problematic for this entire category. Still, if there is proper documentation, it is usually possible to claim ‘supports blood glucose regulation within the normal range,’ ‘supports the actions of insulin,’ ‘supports the metabolism of glucose and the production of energy,’ and so forth,” Clouatre says.
Since a large percentage of diabetes cases are related to diet, exercise and weight status, he also suggests that retailers point clients toward information on these topics. “In fact, it often is easier to talk to customers about diet and energy issues than it is to discuss diabetes, blood sugar, blood pressure or other aspects of the metabolic syndrome,” Clouatre says. He asks people to keep in mind that nutritional approaches to blood sugar control usually take weeks or months to show progress. But these benefits, once achieved, should be fairly stable, so retailers should counsel patience with the use of such supplements.
More tips for promoting or communicating about blood sugar health with your customers come courtesy of Sugarek MacDonald. She suggests renovating the blood sugar health section in your store by making it attractive, interactive and informative for consumers of any age. This may include a cross-merchandised end cap featuring “blood sugar healthy” supplements and packaged foods (including low-glycemic sweeteners like stevia). Also consider providing a basket of fresh fruit and vegetables to address the requirement of five to nine servings per day.
Avoiding product redundancy is important too, Sugarek MacDonald says. For instance, one can pick out three popular blood sugar health supplements to promote on a monthly basis. She also advises retailers to pay attention to their younger customers when it comes to this category. Unfortunately, the increasing obesity problem in young people means more will have to deal with diabetes and prediabetes. It is crucial to advocate a healthy lifestyle before focusing in on supplements, and in this vein, Sugarek MacDonald suggests providing clients with literature or hosting kid-friendly educational seminars about eating healthy and getting daily exercise. WF
References
1. A.M. Belenchia, et al., “Correcting vitamin D insufficiency improves insulin sensitivity in obese adolescents: a randomized controlled trial,” Am. J. Clin. Nutr. 97(4), 774-81 (2013).
2. T.J. Iseli, et al., “Activation of AMPK by Bitter Melon Triterpenoids Involves CaMKKβ,” PLoS One. 8(4), e62309 (2013).
3. Clouatre, et al., “Bitter Melon Extracts in Diabetic and Normal Rats Favorably Influence Blood Glucose and Blood Pressure Regulation,” J Med Food. 14(12), 1496-504 (2011).
4. B.M. Bhat, et al., “Antidiabetic and hypolipidemic effect of salacia oblonga in streptozotocin induced diabetic rats,” J. Clin. Diagn. Res. 6(10), 1685-7 (2012).
5. “Waist Size Linked to Diabetes Risk in Adult Men,” Johns Hopkins Bloomberg School of Public Health, Mar. 17, 2005, http://www.jhsph.edu/news/news-releases/2005/wang-waistsize.html, accessed May 31, 2013.
6. F. Fang, et al., “Vitamin E tocotrienols improve insulin sensitivity through activating peroxisome proliferator-activated receptors,” Mol. Nutr. Food. Res. 54(3), 345-52 (2010).
7. E. Magosso, et al., “Tocotrienols and Nonalcoholic Fatty Liver: a clinical experience,” The Liver Meeting, Poster Presentation No. 672 (Boston 2010).
8. S.K. Jain, “Effect of chromium dinicocysteinate supplementation on circulating levels of insulin, TNF-α, oxidative stress, and insulin resistance in type 2 diabetic subjects: randomized, double-blind, placebo-controlled study,” Mol. Nutr. Food. Res. 56(8), 1333-41 (2012).
9. J. C. Cha, et al., “Nutritional improvement of metabolic syndrome parameters in immature fructose-fed wild-type mice,” Mol. Med. Rep. 4(6), 1053-1059 (2011).
10. S.A. Chacko, et al., “Magnesium supplementation, metabolic and inflammatory markers, and global genomic and proteomic profiling: a randomized, double-blind, controlled, crossover trial in overweight individuals,” Am. J. Clin. Nutr. 93(2), 463-73 (2011).
11. M. Rondanelli, et al., “Key points for maximum effectiveness and safety for cholesterol-lowering properties of plant sterols and use in the treatment of metabolic syndrome,” J. Sci. Food. Agric. [Epub ahead of print] (2013).
12. M. Park, et al., “Depression and risk of mortality in individuals with diabetes: a meta-analysis and systematic review,” Gen. Hosp. Psychiatry. 35(3), 217-25 (2013).
13. A. Eriksson, et al., “Work Stress, Sense of Coherence, and Risk of Type 2 Diabetes in a Prospective Study of Middle-Aged Swedish Men and Women,” Diabetes Care. [Epub ahead of print.] (2013).
Published in WholeFoods Magazine, July 2013


 ingredients below are available from companies interviewed for this piece.
ingredients below are available from companies interviewed for this piece.