These days, dry eye syndrome (DES) is the most common complaint made to eye doctors. It affects 25 to 30 million people, especially women over the age of 40. If you have ever experienced dry eyes, especially while trying to wear contact lenses, you know how important it is to have natural solutions available.
What Is Dry Eye Syndrome?
The typical symptoms of DES include dryness, irritation, grittiness, burning, difficulty reading for extended periods of time and fluctuating blurriness. Excessive tearing and watering are also indicative of DES. In extreme cases, light sensitivity, pain and diminished vision can result. DES is particularly common among peri- and postmenopausal women as there is a gender bias and a hormonal aspect to this syndrome. Additionally, those who have had their gall bladder removed often experience dry eye.
There are two types of dry eye: (1) aqueous insufficiency, which causes a decrease in tear production; and (2) tears that simply evaporate too fast due to lack of oil in the outer layer of the tear film.
Only by restoring proper structure and function to the tear film of the eye can we hope to provide a permanent resolution to DES. After repletion, diet and lifestyle are assessed and addressed, we should consider using remedies like topical lubricant eye drops. However, keep in mind that there is a difference between using natural eye drops and chemical-based artificial tears. Finally, for those so inclined, there is the conventional medical approach of using drugs, corticosteroid eye drops, oral anti-inflammatory drugs and surgical methods (e.g., such as inserting punctual plugs).
The Important Tear Film
The ocular layers that make up the tear film are important to our eyes’ health and for understanding the different characteristics of DES and its common causes. The tear film is shown graphically in Figure 1.
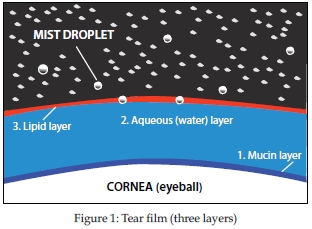
The tear film is made up of three different layers: (1) the mucin or mucus layer, (2) the aqueous or water layer and (3) the lipid or fat layer.
• The mucin layer, which touches the cornea, nourishes the front of the eye. This layer serves as an anchor for the tear film, helping it adhere to the eye, and keeps the eye moist.
• Aqueous secreted by the lacrimal gland forms the middle layer of the tear film, incorporating water-soluble components of the tear film. It provides moisture, oxygen and nutrients to the cornea.
• The lipid layer is produced by the meibomian glands of the eyelids. It is our front line of defense against evaporation, infection, solar radiation and injury to the outside of the ocular surface. It creates a smooth surface for light to pass through the eye. It also keeps the tears from evaporating, maintains the structural integrity of the tear film, and provides a smooth tear film over the cornea when we blink. A recent study reveals that 86% of DES cases involve this layer.
Restoring the Eye’s Structure and Function
Each of these three layers is driven by nutrition. Layers have varying concentrations of vitamins and minerals that promote their proper structure and function. Replenishing the nutrients that saturate ocular tissues is vital for influencing structure and creating proper function. With proper nutrition, vision can be improved and contact-lens wearers will even find a more comfortable fit. Consider that, in the eye, the cornea is two-thirds of its refractive power. If the refracting surface doesn’t have integrity, then good vision is not likely even with glasses or contact lenses. We must nourish all of the layers that make up our tear film.
Each layer has special requirements to do its individual job:
• The mucin layer requires vitamin A (in the form of retinol), which plays a central role in the development of the mucin of the tear film. Vitamin-A deficiency is a cause of goblet cell atrophy and loss of the important, innermost lubricating mucin layer.
• The lacrimal gland’s secretions are promoted by micronutrients like zinc, magnesium and vitamins C, B6 and niacin. Amazingly, the lacrimal gland has hormone receptors in it and tear film is influenced by hormonal fluctuations.
• The oily layer needs essential fatty acids (including omega-3 from flax, fish oils and/or algae, and omega-6 in the form of evening primrose oil, borage oil or black currant seed oil) to create structural integrity in its segment of the three-part layer that makes up the ocular terrain. Also, maintaining an anti-inflammatory diet will support proper eye structure and function.
Zinc is vital in the construction of a healthy corneal surface, having the highest concentration in the entire body in the cornea of the eye and it synergizes well with vitamin A.
If DES goes untreated, it can cause fluctuations in vision, and the cornea can become scratched, scarred and ulcerated. Bioindividuality is key when considering treatment options and DES strategies become complex when we factor in:
• Smoking, which disrupts the way carotenoids are used in the eye and the smoke itself being an irritant exacerbating DES
• Inflammatory, allergenic and/or nutritionally deficient dietary patterns
• Gallbladder surgery and subsequent diminished fat processing
• Gender bias to DES with a predilection to peri- and post-menopausal women
• DES occurring secondary to systemic illnesses such as diabetes or rheumatoid arthritis (RA)
• DES as a result of prescription and over-the-counter drug use.
• DES in post-surgery (Lasik, PRK and cataract) patients
 The Hale Project reported in the Journal of the American Medical Association in 2004 the success of the Mediterranean diet (MeDi) and lifestyle (e.g., non-smoking, moderate exercise, whole foods and a largely plant-based diet) in reducing mortality and morbidity by 50% from all causes after 10 years adherence in individuals aged 70–90 (1). What is good for the body is good for the eyes.
The Hale Project reported in the Journal of the American Medical Association in 2004 the success of the Mediterranean diet (MeDi) and lifestyle (e.g., non-smoking, moderate exercise, whole foods and a largely plant-based diet) in reducing mortality and morbidity by 50% from all causes after 10 years adherence in individuals aged 70–90 (1). What is good for the body is good for the eyes.
Initially a healthy inflammatory reaction helps isolate and protect tissue from further injury so that the body can initiate a healing response. However, an inflammatory response that does not turn itself off upsets the balance in our bodies. Through the modified MeDi, our goal is to limit systemic inflammation by calming unnecessary inflammation signals.
Currently, the most effective treatment for DES we have used is a combination of omega-3 and omega-6 fatty acids, a blend of vitamins A, D, E, C and the cofactors B6, biotin, magnesium and zinc. Getting the materials to the “jobsite” is only half the picture. Transporting them to their optimal location is the rest of the goal. Adding digestive enzymes and healthy bowel bacteria ensures proper digestion and assimilation. Usually within six weeks, the tear film is normal again. If you’ve had gallbladder surgery, use a digestive enzyme containing ox bile to break down the fatty acids you consume.
Gender Bias and DES
More than 60% of women suffer from dry eye at a ratio of nine to one over men, according to WebMD. Peri- and postmenopausal women are some of the most common patient groups affected by dry eye. It is believed that the androgen and estrogen receptors on the cornea and on the meibomian glands, which are tiny oil glands in the eyelids, are involved in the cause.
In a March 2007 study conducted in Bologna, Italy, researchers determined that “Subjective symptoms, tear production and stability, surface dryness and inflammation were significantly related to hormonal fluctuations in the menstrual cycle. In particular, the impairment of these functions appeared to be related to the estrogen peak occurring during the follicular phase, especially in patients with dry eye” (2).
Nutrient Deficiencies and DES
The concept of macro- and micro-nutrient deficiency secondary to systemic disease and its impact on DES is a consideration. DES can accompany systemic diseases like diabetes and RA. DES is exacerbated by prescription and OTC drugs and can also emerge as the result of multiple micronutrient deficiencies that occur as a result of their use. The resulting deficiencies can manifest as ocular disease, visual dysfunction or ocular conditions such as DES.
Those with diabetes have a higher incidence  of DES and are a great example of how certain disease states will require repletion over and above a healthy population. Diabetics typically have about 30% less circulating vitamin C than non-diabetic individuals and less magnesium as well. They are already experiencing greater oxidative stress due to the disease process, and are compromised in vitamins and minerals unless they are supplementing or consistently eating exceptionally well.
of DES and are a great example of how certain disease states will require repletion over and above a healthy population. Diabetics typically have about 30% less circulating vitamin C than non-diabetic individuals and less magnesium as well. They are already experiencing greater oxidative stress due to the disease process, and are compromised in vitamins and minerals unless they are supplementing or consistently eating exceptionally well.
Again, we see the effect of deficiencies or a “cascade effect” associated with systemic disease. A 2006 Indian study published in the journal Ophthalmic Epidemiology found, “Patients with RA in the Indian population have a significantly higher prevalence and severity of dry eye when compared to age- and sex-matched controls” (3).
• Another 2006 study found that flax-seed oil worked to reduce DES equally as well as the oral anti-inflammatory drug Doxycycline prescribed for severe dry eye. Colin C.K. Chan, M.D., speculated at the annual meeting of the American Society of Cataract and Refractive Surgery that the reason may be due to its anti-inflammatory, lipid-modifying properties.
• Often, correcting existing imbalances between omega-3 and omega-6 from animal fat or vegetable oils will alleviate dry eye. Typically, GLA should be taken in an equal ratio to EPA–DHA, in a background of flax oil. Studies report that omega-3 and omega-6 fatty acids in combination result in increased PGE1, which both stimulates aqueous tear secretion and reduces the production of PGE2, which itself acts as an inflammatory agent (4).
• K.A. Trivedi and colleagues at Harvard Medical School in Boston, MA, state, “Women with higher dietary intake of omega-3 fatty acid were at decreased risk of developing DES” (5).
Final Thoughts
We have much at our disposal today in the form of research, healthy dietary options and supplements that can resolve dry eye syndrome. Since most cases of dry eye are due to a deficiency of the oily tear-film layer, replenishing with GLA and maintaining an anti-inflammatory diet is the main natural approach for eliminating dry eye. WF
Katherine Carroll writes for several blogs and magazines, and is the associate editor of NHF’s Health Freedom News. Carroll is a nutritional therapy practitioner and clinic administrator at her and her husband Donn Carroll’s optometry offices.
This article has been reviewed by Donald A. Carroll, OD, NTP
References
1. K.T.B. Knoops, et al., “Mediterranean Diet, Lifestyle Factors, and 10-Year Mortality in Elderly European Men and Women, The HALE Project,” JAMA 292 (12) 1433–1439 (2004).
2. P. Versura, M. Fresina and E.C. Campos, “Ocular Surface Changes Over the Menstrual Cycle in Women With and Without Dry Eye,” Gynecol. Endocrinol. 23 (7), 385–390 (2007).
3. O.S. Punjabi, et al., “Rheumatoid Arthritis Is a Risk Factor for Dry Eye in the Indian Population,” Ophthalmic Epidemiol. 13 (6), 379–384 (2006).
4. D. Wu, M. Maydani and L. Leka, “Effect of Dietary Supplementation with Black Current Seed Oil on Immune Response of Healthy Elderly Subjects,” Amer. J. Clin. Nutr. 70, 536–543 (1999).
5. B. Miljanovic, “Relation between Dietary n-3 And n-6 Fatty Acids and Clinically Diagnosed Dry Eye Syndrome in Women,” Am. J. Clin. Nutr. 82 (4), 887–893 (2005).
Published in WholeFoods Magazine, December 2012