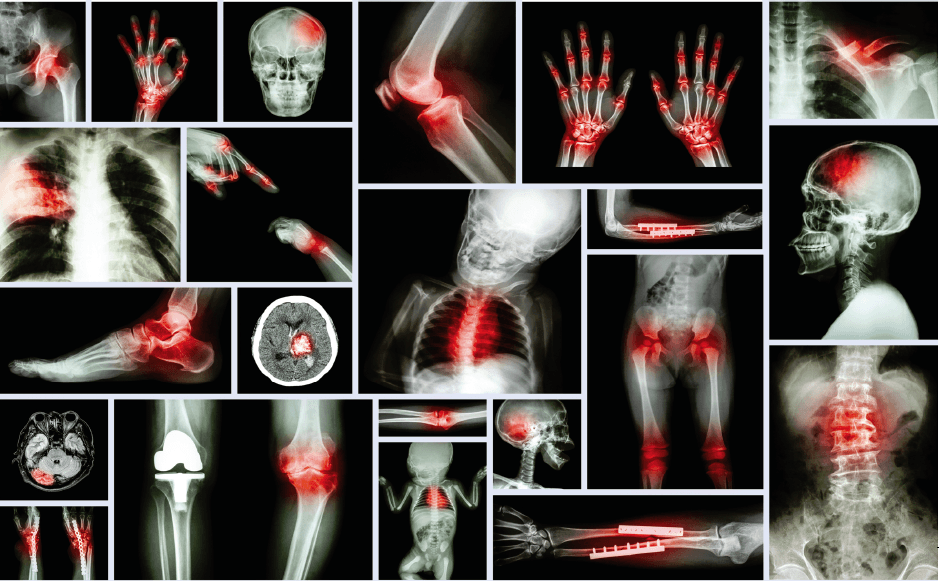
An Inside LookOur bones are continuously being renewed with new bone as old ones break down, thanks to the actions of osteoclasts and osteoblasts. Osteoclasts stimulate acids and enzymes to dissolve minerals and protein in the bone, which in turn breaks down bone, while osteoblasts produce a protein matrix that provides the framework for mineralization (2).
When younger, one’s body can make new bone faster than it can break down — increasing one’s bone mass. However, once peak bone mass is reached, the remolding in the body continues, but more bone is lost than can be gained. Developing osteoporosis depends on the amount of bone mass attained by the time peak bone mass is reached and how rapidly it is lost after that point. The higher the peak bone mass the less likely one is to develop osteoporosis.
The two types of bones in the body that lose mass are: • Trabecular bone — This is the inner portion of the bone that provides structural support to the spongy bone. The trabecular bone provides a reserve of mineral (calcium) that is stored from childhood. When calcium levels are low, the calcium stored in the trabecular bone is used. • Cortical Bone — This is the outer shell of the bone. What Affects Bone Health?
A number of factors can affect bone health. Many factors we can control, while others we cannot. As stated earlier, our age is the number one contributing factor for bone loss but diet is also crucial.
“Diet contributes greatly to bone density as well, and I think that’s something that might not connect with a lot of people when they are younger adults,” says Cheryl Myers, chief of education and scientific affairs for EuroPharma, Inc., based in Greenbay, WI. “We tend to get into a habit of thinking that bones are static, unchanging components of our bodies, and of course, that’s not the case. The body needs to maintain a balance between acidity and alkalinity of the blood. If the blood is too acid, the body releases alkaline minerals from the bone to compensate. What we eat makes a big difference.”
Concurring with Myers, Lauren Stevens, assistant manager, Alta Health Products, Inc., Idaho City, ID suggests, as a good start, consumers need to stay away from heavily processed foods. “Naturally-occurring nutrients are easier for the body to utilize, so consumers should research what foods are rich in which nutrients,” she says. “For example, leafy greens are known to be an excellent source of vegetal silica, but some lettuces typically have more silica content than others.”
As for foods that should be limited or eliminated altogether, Myers suggests, “Sugar, processed meat, soft drinks and grains like bread and pasta [because] these food choices tend to pull calcium from soft tissue and bones.”
In addition to cutting out certain foods that are hazardous to the health of our bones, Steve Holtby, president and CEO, Soft Gel Technologies, Inc., Los Angeles, CA, suggests correcting a nutritional imbalance in our diets. “Over the past 30 years or so, Americans have replaced much of their dietary saturated fat with omega-6 fatty acids,” he explains. “It is estimated that people are now eating 20 times more omega-6s than omega-3s. From a biochemical standpoint, this lopsided imbalance in dietary intake of the omega-6 and omega-3 fatty acids sets the stage for powerful and chronic pro-inflammatory reactions.”
“Coffee, in excess of two cups a day, provides enough acid into the blood to trigger the release of mineral from the bone in order to counter the excess acid load,” says Mark Timon, MS, clinical nutrition, founder and formulator of Vibrant Health, Shelton, CT. “Therefore, one should watch their coffee intake and minimize it as much as possible.”
An uncontrollable risk factor is hormones (3). For women, when reaching menopause, bone loss dramatically increases due to the drop in estrogen. As for men, a low level of testosterone can also cause a loss. Our gender is another cause, but only for women due to having less bone tissue then men (3). Though much research must still be done to find out why, one’s race is also a factor with Caucasians and those of an Asian descent at a greater risk (3). In addition, those with a family history of osteoporosis are placed at a greater risk (3).
“Because agility and mobility can positively affect quality of life as we age,” says Todd Johnson, senior director of marketing, human nutrition and pharma, Balchem/Albion Minerals, Clearfield, UT, physical activity is a “big driver for bone health support.”
“Staying active is important for all kinds of reasons — maintaining weight, fostering a healthy mental outlook, keeping heart and cardiovascular system tuned up — but it is also essential for healthy bones,” says Myers. “Weight-bearing exercise, including short burst exercise like kettlebell lifts, can be of great benefit. The best part is, you can do these exercises for a few minutes, just three days a week and take 20 to 30 minute walks daily, if possible. This will help keep weight in check and strengthen bones without making you feel like you have to join a health club or invest a lot of extra time.”
Researchers have also found tobacco use and excessive alcohol consumption interfere with the balance of calcium in the body to create an increased risk (4). A diet low in calcium — the mineral that makes bones and also helps cells, muscles and nerves work properly — can also contribute to bone loss, fractures and diminished bone density (3).
What Builds Healthy Bones?Calcium.As children, our parents taught us to drink milk to grow strong bones, due to calcium — the most abundant mineral in the body — which is crucial for the development of bones and teeth (5). Calcium is so important, in fact, that the body will absorb calcium from the skeleton to combat a calcium deficiency (5).
Capsules, tablets, or liquids; calcium supplements come in a vast array and are found in dozens of formulations. “The most common form of calcium available is calcium carbonate,” says Holtby. “Calcium carbonate is usually recommended because this form has 40% calcium per tablet, is readily available, and is inexpensive.”
For those low in stomach acid, he recommends the ionized forms of calcium. Chelate and citrate, Holtby says, “tend to be more soluble and have a greater absorption rate. Calcium citrate is much more absorbable than calcium carbonate, but contains only half as much elemental calcium — providing 21% calcium per tablet — and must be taken in larger quantities, resulting in larger pills. Calcium citrate can be used for the elderly and those taking acid-lowering drugs, who may not be able to absorb calcium easily.”
Additional forms of calcium available include phosphate, gluconate, and lactate. Out of these three Holtby says “calcium gluconate and lactate liquid solutions are absorbed in a similar manner and at the same degree as calcium citrate solutions.”
“However, [calcium] is far from the only mineral that people need for healthy bones,” says Myers. “And in fact, too much supplemental calcium is bad for the arteries and the heart.” According to several studies, such as “Calcium Intake from Diet and Supplements and the Risk of Coronary Artery Calcification and its Progression Among Older Adults,” published in the Journal of the American Heart Association in October 2016, researchers found consumers looking to supplement calcium into their diets when food was not enough were more prone to plaque buildup in arteries, which contributed to the risk of a heart attack. Generally, the concern was for supplements that contained calcium only and participants taking between 434 mg and 1,453 mg daily.The newest trend for vitamin D supplementation is toward the D3 form over D2.
Jacob Teitelbaum, MD, a board certified internist, author and a member of EuroPharma’s Science and Education Advisory Board, recommends instead combining calcium with other vitamins and minerals, such as, “Vitamin D, vitamin K and magnesium to make sure calcium is directed into the bones and not into the blood vessel walls.”
Magnesium.Not only is magnesium essential for the absorption and metabolism of calcium, Carolyn Dean, MD, ND and advisory board of the Nutritional Magnesium Association, citing from “The Magnesium Miracle,” August 2017 edition, states how magnesium can “regulate calcium transport, can stimulate calcitonin (hormone) to help preserve bone structure, can suppress parathyroid (hormone) from breaking down bone and converts vitamin D into its active form.”
As with calcium, the majority of magnesium is held in the bone as well as transferred to the blood stream if low and needed. Calcium and magnesium “are usually found together, as the body requires these two nutrients be in a balance, not only for bone health, but for general function,” states Holtby. “[While] calcium acts to help neurotransmission for muscle contraction, magnesium may help to function in an opposite way, for relaxation.”
Dean adds that a 2013 study presented at the annual meeting of the Pediatric Academic Societies in Washington, DC, magnesium’s vital importance was validated within children. According to the study, without magnesium being paired and or balanced with calcium, “magnesium ends up [being] deposited in a child’s kidneys, coronary arteries and cartilage, not in the bones and teeth where it is needed the most.”
Vitamin D.A fat-soluble vitamin found in foods such as fatty fish, cheese and in fortified foods, like milk, vitamin D also plays an important role in supporting bone health. With adequate amounts, vitamin D “acts like a hormone in the body and helps the body to increase absorption of calcium and other minerals,” states Holtby.
Without vitamin D, bones can become thin, brittle and even misshapen. A vitamin D deficiency can also cause osteomalacia in adults and the development of rickets in children. According to the National Osteoporosis Foundation, the recommended amount for women and men under the age of 50 is 400 – 800 international units (IU) daily and for those age 50 and older 800 – 1,000 IU daily is recommended.
There are two forms of Vitamin D: ergocalciferol (Vitamin D2) and cholecalciferol (Vitamin D3). While Vitamin D2 is made by plants in response to UV radiation, Vitamin D3 is made when the human skin is directly exposed to enough sunlight.
Currently the newest trend for vitamin D supplementation “is toward the D3 form over D2 despite the ample evidence that at physiological doses they are equally effective,” said Neil E. Levin, CCN, DANLA, senior nutrition education manager, NOW Foods, Bloomingdale, IL. However, the turn toward Vitamin D3 may be due to many of us not receiving “the level of vitamin D3 we need through our diets or exposure to sunlight,” states Myers. “In fact, anyone living in a northern climate, working indoors most of the year, or who has darker skin, probably needs a supplemental source.”
According to a study published in the Journal of Clinical Endocrinology, another reason for the turn to Vitamin D3 may be due to potency. In the study, scientist accessing 33 healthy adults, who for 11 weeks were taking either vitamin D2 or D3, found vitamin D3 to be 87% more potent at raising and maintaining blood levels and to also produce 2 to 3 times greater storage of the vitamin than D2 (6).
Vitamin K2.This nutrient’s “ability to direct calcium to where it needs to go, especially to the bones and not soft tissues,” states Audrey Ross, ND, western regional educator, Country Life Vitamins, Hauppauge, NY, is what makes vitamin K2 an important player within bone health. The fat-soluble vitamin is “necessary for the proper synthesis of osteocalcin, a protein hormone made by osteoblasts and believed to be essential for the building of bone, says Timon “Epidemiological studies of patients with and without osteoporosis indicate that vitamin K2, usually obtained from certain fermented foods, is most critical to the synthesis of osteocalcin with an activity far superior to vitamin K1, the form commonly found in plants.”
As for why vitamin K2 is perceived as superior to vitamin K1 , Sky Garmon, marketing associate, Jarrow Formulas, Los Angeles, CA states “Vitamin K2 is ten times better absorbed than K1, found in spinach, and is responsible for the carboxylation of specific bone proteins needed for building bones.” In addition, vitamin K2, when combined with vitamin D3, helps to inhibit osteoclasts — a cell responsible for breaking down bone tissue (7).
In a study presented at the International Conference on Children’s Bone Health in Wurzberg, Germany, a group of 20 children between the ages of 5 – 15 with clinically confirmed fractures were compared to a control group of 19 children ages 7 – 17 who had no fractures. The study revealed the children with bone fractures had lower vitamin K2 in their systems compared to the control who had 2 times greater.
Collagen.Besides the usual minerals and vitamins, Dean, also suggests taking “collagen, the most abundant protein in the body, [which] makes up about 90% of the bone matrix.” The bone matrix contains protein and magnesium and provides the bone with its flexibility and resistance to brittleness. “When building new bone, osteoblast cells first make a bone collagen matrix called osteoid. Then minerals are added to the collagen framework,” which then gives the bone its flexibly and ability to absorb impact, adds Richard Passwater Jr., product education director for Bio Minerals, a specialty line from Natural Factors, based in Monroe, WA.
In addition, Passwater says, “Bone collagen fibers serve as a template, or the ‘binding sites’ or ‘parking spaces,’ for bone minerals such as calcium and phosphorous. A rich, multi-directional one collagen fiber network creates plenty of surface area or places for calcium and other minerals to bind to so a person has great bone mineral density (BMD) potential. As the collagen network in bone decreases so does the BMD potential.”
A recent double-blind placebo-controlled clinical study on the effects of osteoarthritis on joint function, found 94 osteoarthritis-diagnosed women who took 8 g of Peptan Collagen Peptides for six months had significantly lower pain and better joint flexibility at the end of the study, than the control group who were taking a placebo (8).
Silica. Another helpful nutrient for bone density is silica, a trace mineral that is found in bones, teeth, the skin, eyes, glands and organs. When choosing a silica supplement, Stevens believes choosing an “herbal or vegetal silica rather than mineral silica,” is best due to “mineral silica having a decalcifying effect upon the bones.”
Vitamin C.Although few trials have tested the efficacy of vitamin C supplementation for bone health and fractures risk, vitamin C is a required “cofactor to activate most of collagen building,” states Passwater. Specifically vitamin C helps in the process of hydroxylation of lysine and proline during collagen synthesis by way of osteoclasts. In one double-blind, placebo-controlled trial of 60 osteopenic women, ages 35 – 55, patients taking a mixture of calcium, vitamin D and a CB6Pro (500 mg vitamin C, 75 mg vitamin B6, and 500 mg of proline) daily for one year were found to have no bone loss in the spine and femur versus those taking simply calcium and vitamin D (9).
Boron. By helping to facilitate calcium directly into the bones, boron too can help prevent porous and weak bones. Boron has also been shown to regulate estrogen, which can also protect the density of bones. “Adequate boron elevates levels of key hormones required for the deposition of calcium into bone tissues,” states Timon. “Testosterone, estradiol, DHEA and calcitiolall are elevated and maintained at optimal levels within an indiviual with enough boron. Human clinical trials have shown that negative calcium balance (i.e., the loss of more calcium through the urine than is absorbed across the intestinal mucosa) is halted within 24 hours when adequate boron is included in the diet.”Sugar, processed meat, soft drinks and certain grains tend to pull calcium from soft tissue and bones.
Vitamin B6, vitamin B12 and folic acid are three ingredients along with zinc that can help metabolize homocysteine and control its pro-inflammatory effects,” said Timon. “Subclinical deficiencies of one or more of these nutrients are often tied to bone deterioration.”
HerbsHorsetail.This herb is a plant source rich in silica, that is beneficial to collagen production. “While this herb is not safe for consumption in its raw form, after properly prepared it produces one of the highest concentrations of vegetal silica,” states Stevens. “Humans [are] born with extremely large amounts of silica pulsing through their bodies due to its role in building bones, connective tissues, collagen, nails and hair. Levels of this key nutrient decline as we age, but maintaining a diet rich in vegetal silica and supplementing with an herbal silica supplement can…thusly lead to a stronger skeletal structure, keeping a full head of hair and reducing signs of aging, among many other amazing bodily benefits.”
Cat’s Claw.According to the University of Maryland Medical Center, the bark and root of this woody vine contains antioxidant properties that have been suggested for those with rheumatoid arthritis (RA) because they may reduce inflammation. One small randomized, double-blind study published in the Journal of Rheumatology found 40 people suffering from RA were able to reduce joint swelling and pain 50% more using cat’s claw than a placebo.
Quercetin.A flavonoid, found in fruits and vegetables, quercetin is an anti-inflammatory that acts as an antioxidant, fighting the natural process of oxidation that takes over as we age. In a 28-day study of post-menopausal women, published in the journal Phytomedicine, a fixed combination of plant extracts, which included quercetin resulted in an up-regulation of the bone protein BMP-2 and COL1A1 gene (provides instructions for making part of type I collagen) which are linked to bone and collagen formation while down- regulating genes linked to osteoclastogenesis (10).
Nettle.According to the Milton S. Hershey Medical Center the leaves and stems of nettle have been used throughout history in traditional medicine to treat arthritis and relieve sore muscles. Nettle is typically applied topically at the site of pain, but has also been used orally in a few studies. One particular study, published in the December edition of the Journal of Rheumatology, found stinging nettle able to inhibit the inflammatory cascade in autoimmune diseases such as rheumatoid arthritis (11).
Red Clover.Red clover is a natural provider of “isoflavones, which have a chemical solution that is not unlike the estrogen found in humans,” said Trisha Sugarek MacDonald, BS, MS, Sr. director of research and development, national educator, Bluebonnet Nutrition Corporation, Sugarland, TX. Because estrogen levels drop in women during menopause, the risk of developing osteoporosis significantly rises. However, recent “research has shown that dietary intake of isoflavones may help maintain hormonal health by binding to the same receptors estrogen utilizes, and therefore aiding in bone health,” adds MacDonald. “In 2004, a study in the February edition of American Journal of Clinical Nutrition found that women taking red clover isoflavones had significantly slower spinal bone loss compared with women in the placebo group.”
In another study published in 2015 of the July edition of Evidence-Based Complementary and Alternative Medicine, 60 menopausal women taking a daily dose of 150 ml of a red clover extract containing 37.1 mg of isoflavones for 12 weeks, saw improvement in their bone health when compared to a placebo (12).
Additional herbs that may be beneficial include green tea, ginger, turmeric, holy basil, chamomile, Chinese goldthread, barberry, Baikal skullcap, Hu zhang (Japanese knotweed), rosemary, hops, feverfew and oregano. As always, consult with a physician before starting any herbal supplementation.WF
References
- National Institute of Arthritis and Musculoskeletal and Skin Diseases, “Osteoporosis: Peak Bone Mass in Women,”www.niams.nih.gov/Health_Info/Bone/Osteoporosis/bone_mass.asp, accessed Dec. 20, 2012.
- Office of the Surgeon General (US). Bone Health and Osteoporosis: A Report of the Surgeon General. Rockville (MD): Office of the Surgeon General (US); 2004. 2, The Basics of Bone in Health and Disease.Available from: https://www.ncbi.nlm.nih.gov/books/NBK45504/
- Mayo Foundation for Medical Education and Research. “Bone Health: Tips to Keep Your Bones Healthy,” http://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/bone-health/art-20045060?pg=1, accessed July 3, 2017.
- National Institute of Arthritis and Musculoskeletal and Skin Disease, “Smoking and Bone Health,” https://www.niams.nih.gov/Health_Info/Bone/Osteoporosis/Conditions_Behaviors/bone_smoking.asp, accessed July 3, 2017.
- Oregon State University Micronutrient Information Center, “Calcium,” http://lpi.oregonstate.edu/mic/minerals/calcium, accessed July 3, 2017.
- Robert P. Heaney,et al., “Vitamin D3 Is More Potent Than Vitamin D2 in Humans,” The Journal of Clinical Endocrinology & metabolism (2011) 96 (3): E447-E452 available: https://academic.oup.com/jcem/article-lookup/doi/10.1210/jc.2010-2230
- Today’s Dietitian, “Vitamin K2 – A Little-Known Nutrient Can Make a Big Difference in Heart and Bone Health, http://www.todaysdietitian.com/newarchives/060113p54.shtml, accessed July 3, 2017.
- J.X. Jiang, et al., “Peptan Collagen Peptides for Treatment of Knee Osteoarthritis: A Double-Blind, Randomized, Placebo-Controlled Study”, Agro Food Industry Hi Tech 25(2), 20–21 (2014) available: https://cdn.shopify.com/s/files/1/0261/0659/files/PrimalPeptides_ClinicalStudy.pdf
- Masses PG, et al., “Enhancement of calcium/vitamin d supplement efficacy by administering concomitantly three key nutrients essential to bone collagen matrix for the treatment of osteopenia in middle-aged women: a one year follow-up.”Journal of Clinical Biochemistry and Nutrition 46 (1), 20-9 (2010) Available: https://www.ncbi.nlm.nih.gov/pubmed/20104261#
- Yumei Lin, et al., “Bone Health Nutraceuticals alter microarray mRNA gene expression: A Randomized Parallel, Open-Label Clinical Study,” Phytomedicine 23 (1), 18-26 (2016) Available: http://www.sciencedirect.com/science/article/pii/S0944711315003669
- Klingelhoefer S, et al., “Antirheumatic Effect of IDS 23, a Stinging Nettle Leaf Extract, on in Vitro Expression of T Helper Cytokines,” Journal of Rheumatology 26 (12), 2517-2522 (1999) Available: https://www.ncbi.nlm.nih.gov/pubmed/10606356
- Thorup, Anne Cathrine et al. “Intake of Novel Red Clover Supplementation for 12 Weeks Improves Bone Status in Healthy Menopausal Women.” Evidence-based Complementary and Alternative Medicine : eCAM2015 (2015): 689138. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4523657/