Fact or fiction: Bones are mainly “calcium sticks,” developed until the teen years and frozen until they become brittle from old age.
No way! Set the record straight in your store with some basic education about how bones evolve throughout our lives and the role nutrition plays in this process. After all, bone health is not just a concern for the young and the elderly. Everyone needs to factor bone support—and joint care—into their overall wellness plan so they can move fluidly and comfortably throughout life.
This month, WholeFoods Magazine is kicking off its five-part bone and joint series with a discussion about bone strength and the topic will build from here. Stay tuned for devoted bone/joint features on issues such as bone flexibility, cartilage support, inflammation support for joints and joint care for athletes, all running from now until October.
Why Me?
When bone density results indicate that there could be a problem, shoppers may ask, “Why me? I’m healthy!” The answer is complex, as numerous factors contribute to bone strength and density—some we can control and others we cannot.
Uncontrollable risk factor number one is one’s gender. “Women are more likely to develop osteoporosis than male counterparts,” states Chris D. Meletis, N.D., naturopathic physician, www.DrMeletis.com.
Gender combined with aging—another factor we cannot control—has a huge effect on our skeletal  system. “In women, the bone-building process is nearly complete by age 17,” says Michael T. Murray, N.D., director of product science and innovation, Natural Factors Nutritional Products, Inc., Monroe, WA. This “glory period” only lasts about a decade, as women lose about 0.4% of bone mass in the femoral neck every year after the age of 28.
system. “In women, the bone-building process is nearly complete by age 17,” says Michael T. Murray, N.D., director of product science and innovation, Natural Factors Nutritional Products, Inc., Monroe, WA. This “glory period” only lasts about a decade, as women lose about 0.4% of bone mass in the femoral neck every year after the age of 28.
The situation worsens after menopause, according to Murray. “After menopause, the rate of loss is faster, with an average 2% loss annually during the first five to 10 years. Bone loss continues in older women past age 70, but at a much slower rate,” he states.
Around this time is when there is a shift in how the body uses key bone minerals. Nena Dockery, technical services manager at Stratum Nutrition, St. Charles, MO, explains that “as part of the aging process, the body begins to reabsorb more calcium and phosphate from the bones than is maintained within the bone for new bone formation. This weakens the bone and eventually results in osteoporosis.”
This happens because, as a natural part of aging, osteoclast cells remove weakened bone faster than osteoblasts can replace it, states Marci Clow, M.S., RDN, senior nutritionist at Rainbow Light, Santa Cruz, CA, putting older adults at risk of fracture.
Add family history, having a small build and being of Asian or European descent to the list of risk factors we cannot help. One’s build may come as a surprise, but the reason why is that “if you have a smaller frame, you are more likely to have weaker bones, all things being equal, as you bear less weight when exercising,” Meletis explains. Doing weight-bearing exercises supports healthy bone building.
Other contributors to bone health are more within our control.
And, because some bone-support contributors are highly achievable, it is important to remind consumers they can support their skeletal system life.
Bone is living tissue that is constantly remodeling thanks to the actions of osteoclasts and osteoblasts. According to Murray, osteoclasts stimulate the formation of acids and enzymes that dissolve minerals and protein in the bone; this action breaks down bone, which is a normal process.
Meanwhile, osteoblasts produce a protein matrix made mainly of collagen, which provides the framework for mineralization.
“Bone remodeling is normally a balance of bone resorption and bone formation,” Murray states. “An imbalance between bone removal and bone replacement results in bone loss.”
 One factor that can tip the balance is osteocalcin, an important protein in the bone matrix that is made by osteoblasts. According to Eric Anderson, global vice president of sales and marketing at NattoPharma USA Inc., Metuchen, NJ, osteocalcin cannot be made without sufficient vitamin K levels. Osteocalcin is released during bone resorption and is “responsible for monitoring the healthy balance of bone remodeling—ensuring osteoclastic activity (bone breakdown) does not exceed osteoblastic activity (bone buildup),” he states.
One factor that can tip the balance is osteocalcin, an important protein in the bone matrix that is made by osteoblasts. According to Eric Anderson, global vice president of sales and marketing at NattoPharma USA Inc., Metuchen, NJ, osteocalcin cannot be made without sufficient vitamin K levels. Osteocalcin is released during bone resorption and is “responsible for monitoring the healthy balance of bone remodeling—ensuring osteoclastic activity (bone breakdown) does not exceed osteoblastic activity (bone buildup),” he states.
When osteocalcin is activated by vitamin K, it “binds calcium in the bone matrix, gradually leading to increased bone mineral content, and thus leading to more resistance and less susceptibility to fracture,” he continues.
When vitamin K intake is insufficient, Anderson says osteocalcin cannot do this important job. Nutritional deficiencies and the possible role of supplementation with nutrients like vitamin K for bone health will be discussed in the next section.
So, what else affects bone strength?
Lack of exercise, poor diet, taking certain medications, various health conditions, smoking and drinking alcohol in excess can also affect the skeletal system, as can hormonal issues. Meletis states, “Low sex hormones increase risk of osteoporosis for both males and females. Excess thyroid hormone levels can lead to weaker bones, and if you have overactive adrenal glands producing too much cortisol/cortisone or a parathyroid condition, this can also accelerate bone loss.”
Stomach acid, says Bruce Topping, educator for Garden of Life, Palm Beach Gardens, FL, also can affect the bones. Low levels—either naturally occurring or induced by acid blockers—can be problematic. “Without stomach acid, it is very difficult to properly utilize protein and minerals from our food,” he states, and the body may not be able to make full use of the nutrients one consumes.
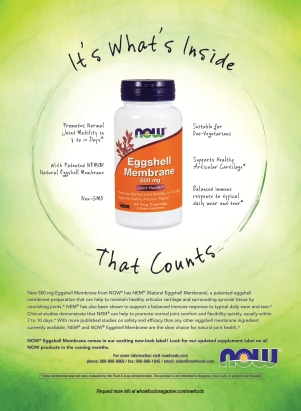
Neil E. Levin, CCN, DANLA, nutrition education manager at NOW Foods, Bloomingdale, IL, says low stomach acid is especially problematic for older individuals.
At the end of the day, shoppers truly need education about all bone health factors and whether they  should consider talking to their physicians about extra nutritional support. According to Dallas Clouatre, Ph.D., consultant for R&D at Jarrow Formulas, Inc., Los Angeles, CA, only about half of individuals suffering from osteoporosis are aware of their condition. “On the National Health and Nutrition Examination Survey (NHANES), only 1% of men and 11% of women over 65 reported that they had osteoporosis,” he explains. “However, bone mineral density (BMD) testing revealed that 4% of male and 26% of female survey takers actually had the disease. The mismatch between perception and reality with regard to bone health gains importance from the fact that the number of individuals involved is huge.”
should consider talking to their physicians about extra nutritional support. According to Dallas Clouatre, Ph.D., consultant for R&D at Jarrow Formulas, Inc., Los Angeles, CA, only about half of individuals suffering from osteoporosis are aware of their condition. “On the National Health and Nutrition Examination Survey (NHANES), only 1% of men and 11% of women over 65 reported that they had osteoporosis,” he explains. “However, bone mineral density (BMD) testing revealed that 4% of male and 26% of female survey takers actually had the disease. The mismatch between perception and reality with regard to bone health gains importance from the fact that the number of individuals involved is huge.”
King Calcium
Poor dietary choices were noted as a contributor to bone health problems, which can lead to deficiencies in key bone health nutrients. “So, I would say that one of the most ‘fixable’ factors that can lead to bone loss is lack of calcium intake,” says Clow.
Clow says calcium is deposited and withdrawn daily in the bones “like money in a bank…so, investing in your bone health early in life, could be of great benefit to the future of your bones.”
Calcium gives structure and strength to skeletal tissue, she explains. Clow believes that we should try to get the calcium we need from dietary sources, and then turn to supplements when diet is not enough.
This might be nearly everyone, says Jason DeWitt, managing partner at Coral LLC, Carson City, NV: “Our foods and vegetables are mineral and nutrient depleted due to unsustainable farming practices, supplementation is almost inevitable.”
There are numerous forms of supplemental calcium available, but which is best?
Erin Stokes, N.D., Megafood medical director, FoodState, Manchester, NH, prefers options that are minimally processed and sourced from nature: “I believe it is best to get calcium in a variety of forms, just as it exists in nature and in food.”
 Dockery says calcium carbonate is naturally found in limestone, oyster shells, algae and eggshells, and contains the highest amount of elemental calcium (35–40% calcium), allowing for smaller doses. Her favorite source is eggshell because it does not cause gastric distress and, for those concerned about heavy metal content, “ESC brand calcium from eggshells is naturally virtually lead-free (50x lower than Prop 65 approved levels).”
Dockery says calcium carbonate is naturally found in limestone, oyster shells, algae and eggshells, and contains the highest amount of elemental calcium (35–40% calcium), allowing for smaller doses. Her favorite source is eggshell because it does not cause gastric distress and, for those concerned about heavy metal content, “ESC brand calcium from eggshells is naturally virtually lead-free (50x lower than Prop 65 approved levels).”
Underscoring this point, Murray agrees it is important for those who want to take calcium carbonate to find something that does not have high lead levels, which can be the case in some inexpensive versions of the supplement made of materials like oyster shell.
Topping also likes plant-based calcium for its purity and the additional minerals that occur naturally with it. “The nice thing about using plant forms is that they’re made up of many minerals, including trace minerals,” he states. “In my opinion, the best raw material is called ‘AlgaeCal’ and is currently the only certified organic plant calcium available and has been clinically studied.”
Another vegetarian source of bioavailable calcium that is naturally found with a variety of minerals—more than 70 in total— is red algae-derived Aquamin (Marigot, Ltd.), which is harvested in the arctic waters of Iceland. States Levin, “Research indicates that this seaweed-derived multimineral complex may support proper bone mineralization and help to regulate key factors involved in the normal immune system response to typical joint usage.” He says this calcium form provides “almost double the calcium (percentage-wise by weight) as a typical mineral chelate like calcium citrate.”
Wild oregano also makes a good plant-based source of calcium. According to information provided by North American Herb and Spice Co., “Ground, wild oregano provides some 30 mg of calcium per teaspoon. Two teaspoons thus amount to approximately 6% of the daily requirement. Few other foods have such a density.”
The company points out that wild oregano and rosemary are rich sources of vitamin K. “A mere
|
Bone Health Vocab 101 Bone remodeling: The process of breaking down old bone and rebuilding it. Bone resorption: The removal of bone tissue by osteoclasts. Calcitonin: A hormone that lowers calcium and phosphate blood levels and promotes bone formation. Osteoblasts: Cells that build new bone by producing a matrix that becomes mineralized. Osteocalcin: Protein made by osteoblasts in the presence of vitamin K. Found in the bone matrix. Osteoclasts: Cells that “nibble away” at old bone and are responsible for resorption. Osteoporosis: Condition that causes bones to become weak and brittle. |
teaspoon of ground oregano contains 11 mcg of the vitamin, nearly 9.5% of the daily requirement for men and 12.5% for women.”
Tricalcium phosphate is another form to consider for those interested in taking calcium with other minerals. Murray says, “Tricalcium phosphate provides three molecules of calcium for every molecule of phosphorus, making it a highly efficient source of both calcium and phosphorus.”
This is important because phosphorus is essential for strong bones, yet half of North American women are phosphorus deficient, according to Murray. He adds, “Clinical studies indicate that consuming calcium with phosphorus in the form of tricalcium phosphate is more effective at building strong bones than consuming calcium alone.”
Other calcium forms are also helpful for offering full-spectrum bone support. Meletis says coral calcium and calcium hydroxyapatite deliver other bone and mineralization constituents for bone nourishment when processed correctly. One study compared the absorption of coral calcium with calcium carbonate and found the coral form was better absorbed (1).
Finding a form that is absorbable (and taking the proper companion nutrients to aid its absorption and breakdown) may also be a concern for shoppers, but this issue is not as straightforward as it may seem.“There are surprisingly few conclusive studies proving superiority and bioavailability of one form of calcium over another,” Clow says. In addition, several variables complicate the calcium absorption situation like age, environmental and dietary conditions and race (2).
|
Calcium Supplementation: Still a Necessity - Safety in Question Calcium definitely plays a a vital role in bone health, but how much is too much? Click here for a whitepaper from Albion Nutrition reviewing several studies on the safety of calcium supplementation. |
|
Dockery says eggshell calcium falls in the “readily absorbed” camp. Several other options also said to offer good absorption include high elemental calcium forms like dicalcium malate and calcium bisglycinate, says Daniel Heller, N.D., senior scientific affairs associate for Life Extension, Fort Lauderdale, FL. He also likes a patented chelated compound of calcium and hydrolyzed collagen peptides (KoAct from AIDP) “designed to enhance collagen support and turnover while supporting optimal bone mineral density and strength.”
DeWitt calls coral minerals “a perfect body-friendly nutrient.” He says they are “predigested” by polyps from the sea, making them easy to digest and absorb, and “the mineral complex perfectly resembles our natural bone structure…Coral minerals supply all mineral cofactors necessary for optimal absorption.”
Levin says individuals with low stomach acid levels may have trouble digesting calcium from food and non-chelated forms. He says predigested supplemental forms that might work well for these individuals include citrate, malate or ascorbate calcium or bonded calcium to specific amino acids. “All are weak low-molecular weight acids that form a stable bond with the alkaline calcium,” he explains. “The resulting compound simulates the calcium complexes formed naturally during proper digestion.”
Meanwhile, those with low hydrochloride (HCl) production may want to look for a calcium supplement with added betaine HCl, says Clow.
 Clouatre adds that bone-derived calcium (a.k.a. ossein-hydroxyapatite complex or microcrystalline hydroxyapatite) is a worthy calcium form to try since it often performs well in absorption tests. He says clinical studies have found 5% additional calcium in the spinal vertebrae of women taking bone-derived calcium rather than calcium carbonate, which might be attributed to the actions of the other components found in the calcium and not just the calcium itself.
Clouatre adds that bone-derived calcium (a.k.a. ossein-hydroxyapatite complex or microcrystalline hydroxyapatite) is a worthy calcium form to try since it often performs well in absorption tests. He says clinical studies have found 5% additional calcium in the spinal vertebrae of women taking bone-derived calcium rather than calcium carbonate, which might be attributed to the actions of the other components found in the calcium and not just the calcium itself.
But, retailers should be careful how they present this info to shoppers; calcium absorption is complicated, as noted.
Clouatre says in the end, there is not much difference in absorption among the various calcium forms when people with normal stomach acid function take them with food. “If taken with meals, most forms of calcium yield similar absorption data and the differences between the best and the poorest performing sources can generally be overcome by taking just a bit more calcium,” he states.
Clouatre provides average (mean) absorption for various calciums calculated based on three to eight studies (for each of four calcium salts) and 12–14 studies (for carbonate and milk calcium):
• carbonate, from 26.4% (fasting) to 29% (meal)
• citrate/malate, from 32% (fasting) to 37% (meal)
• citrate, 23.5% (fasting)
• lactate/gluconate, 24.5% (fasting)
• chloride, 30.6% (fasting)
• milk, 32.4%, cheese, 32.8%
• mineral waters, 32.3%
|
Select Bone Strength Support Supplements
Interviewees were asked to share their top-selling bone health supplements, and here’s what they had to say: Coral LLC: Coral Energy drink, Coral Alkaline Water Sachets, Ecopure Coral Powder and Coral White toothpaste. Garden of Life: Raw Calcium and Organic Plant Calcium. Jarrow Formulas: Bone-Up, Ultra Bone-Up, Bone-Up Three Per Day, JarroSil. Life Extension: Bone Restore, Bone Restore with KoAct and Bone Restore with Vitamin K2. MegaFood: Full line of whole food multivitamins for every stage of life. NattoPharma USA Inc.: Raw material MenaQ7, a natural vitamin K2 MK-7. Found in finished products such as SuperNutrition’s SimplyOne Heart Smart and MK-7 featuring MenaQ7 from Doctor’s Best. Natural Factors Nutritional Products, Inc.: BioSil Beauty, Bones, Joints; BioSil Healthy Bones Plus; Whole Earth & Sea Bone Structure Multivitamin & Mineral. Natural Vitality: Natural Calm Plus Calcium, Osteo Calm. North American Herb and Spice Co.: BoneActiv, Oregano P73 products. NOW Foods: NOW Bone Calcium tabs and Bone Strength tabs; NOW Full Spectrum Minerals; NOW Red Mineral Algae is a source of Aquamin; NOW Cal-Mag DK Caps; NOW MK-7 Vitamin K-2 derived from natto. Rainbow Light: Food-Based Calcium, OsteoBuild, Calcium Citrate Mini-Tabs, Calcium Citrate Chocolate Chewable, Everyday Calcium and Magnesium Calcium+. Stratum Nutrition: ESC brand calcium from eggshells (raw material). Trace Minerals: Complete Cal/Mag 1:1, Coral Calcium with ConcenTrace, Liquid Cal/Mag/Zinc, Liquid Coral Calcium, Liquid Vitamin D, Liquid Magnesium, Magnesium Tablets, Mega-Mag, Ionic Boron. |
|
He states, “Although these numbers must be interpreted cautiously inasmuch as the studies were performed using different test groups and study parameters, it is clear that when averaged over several studies, calcium absorption is limited to about one-quarter to one-third of ingested dose with the greatest documented differences between calcium forms amounting to only a few percent.”
Murray feels that what makes the most difference in calcium supplementation are the other nutrients consumed alongside it. This is perhaps the most important point you can make to shoppers that are interested in bone health. And, taking large amounts may not be necessary for most healthy adults. “There is no reason to take more than 1,000 mg per day of calcium as a supplement,” he believes. “Studies are clear: the benefits seen at 2,000 mg per day are not greater than those seen with 1,000 mg.”
Even taking 1,400 mg a day of calcium may be problematic, according to a long-term study of Swedish women (3). “Every vitamin or mineral has an optimal intake level range. When a nutrient is taken in very high amounts by itself, this is where we see potential problems,” says Stokes.
Splitting calcium doses might be helpful, too.
Too much of a good thing?
As vital as calcium may be for maintaining healthy bones and teeth, many sources feel taking too much calcium can have negative repercussions. First, Topping says calcium taken without co-factor minerals and fat-soluble vitamins usually will not improve bone mineral density. Second, he states, “Several large controlled studies have raised alarms about high blood calcium and the potential increase in cardiovascular disease risk.”
A 2011 study from British Medical Journal published a meta-analysis based on five clinical trials that included a total of over 8,000 people. The analysis found that calcium supplements may increase the risk of cardiovascular events, including heart attack (4).
Anderson offers some information for why this might be the case: “[Calcium] has a natural affinity for depositing in arteries, where it hardens into an immovable plaque. This plaque drastically reduces arterial flexibility, and arteries need to be flexible to allow an ease of blood flow to and from the heart.”
He adds that most women do not keep track of exactly how much calcium they consume, be it from supplements, food or calcium-fortified products. For this reason, Anderson believes shoppers should be coached to take additional nutrients that help metabolize this bone support mineral.
But, there may be some subtleties to consider. On the flip side, Heller and Levin cite a large study suggesting that high-dose calcium supplements may not automatically put people at risk of heart issues. “Data was examined from the Nurses’ Health Study (1984-2008) and showed the relative risk of cardiovascular disease for women taking calcium supplements at a dose of at least 1 g per day was 18% lower than for women not taking supplements, and the risk of coronary heart disease was 29% lower,” he states. The research was published in 2014 and involved more than 74,000 women (5).
Clouatre believes that when one takes higher quantities of a calcium form that includes its natural cofactors, there may be less of a danger to cardiovascular health than when people take highly purified calcium in isolation.
Join the Party
So, if shoppers want to make sure their calcium intake is maximized to the fullest, share this advice: take calcium with other important bone support nutrients.
“Calcium is not a stand-alone element for bone health,” says Ken Whitman, president of Natural Vitality, Austin, TX. “It needs to be part of a ‘soup’ that includes magnesium, vitamins D3, K2 and boron. Many people have been taking calcium supplements for years on the advice of doctors and you’ll notice that the osteoporosis and brittle bone epidemic is still with us.”
Vitamin D is key for supporting bone health because it promotes calcium and phosphorus absorption by simulating bone calcium mobilization. Vitamin D converts to an active form in the body called 1,25-dihydroxyvitamin D [1,25-(OH)2D] or calcitriol. This active form “regulates the transcription of a number of vitamin D-dependent genes coding for calcium-transporting proteins and bone matrix proteins” (5).
To emphasize this point, Murray says that data from the Women’s Health Initiative study of more than 36,000 postmenopausal women suggest taking a combination of 1,000 mg/day of calcium and 400 IU/day of vitamin D decreased the risk of hip fractures by 12% when compared with placebo (6). Women who took these supplements at least 80% of the time experienced a 29% decreased hip fracture risk over the placebo group. “That is a significant amount especially with vitamin D having been supplemented at levels now known to be less than ideal,” he believes.
Clouatre notes that adequate vitamin D and magnesium intake and blood levels are associated with better cardiovascular health.
On the magnesium front, experts say this mineral is vital to bone health and other aspects of wellness, including as a companion for calcium. “Magnesium keeps calcium dissolved in the blood. Without the proper balance of magnesium to calcium, about a 1:1 ratio, calcium ends up depositing in kidneys and can create kidney stones, in coronary arteries where it can lead to clogged arteries, and in joint cartilage, rather than in bones where we need it most,” said Carolyn Dean, M.D., N.D., magnesium expert and medical director of the nonprofit Nutritional Magnesium Association in a recent press release (4). At the very least, individuals should not consume more than a 2:1 ratio of calcium to magnesium.
According to Clouatre, healthy bones are made of approximately 1.2–1.8% magnesium; those with osteoporosis may only have 0.5–0.6%. Interestingly, Guy Abraham, M.D., a research gynecologist and  endocrinologist, found evidence implying that women with osteoporosis also have a deficiency in calcitonin. In these women, this hormone (which promotes bone formation) is only made when twice as much magnesium as calcium is consumed.
endocrinologist, found evidence implying that women with osteoporosis also have a deficiency in calcitonin. In these women, this hormone (which promotes bone formation) is only made when twice as much magnesium as calcium is consumed.
But even in good health, people should think about their intake ratio. Whitman explains that consuming too much calcium depletes magnesium in the body, “so retailers would be advised to ask customers who are purchasing calcium supplements if they are also making sure they are keeping their magnesium levels in balance.”
In fact, Murray goes so far to say that an imbalance in these minerals—where people take too much calcium and too little magnesium—may actually be a reason why excess calcium intake is linked to heart issues in some studies.
So, how exactly does magnesium help? According to Whitman, the mineral activates vitamin D and helps with the assimilation of calcium. He states, “Calcium alone makes bones brittle (think of dropping blackboard chalk on the ground) but magnesium makes them pliable.”
Shoppers’ understanding of the role of vitamin D and magnesium for bone health is broadening, but other important nutrients are still falling under the radar. Circling back to phosphorus, this mineral is essential for bone support, but retailers need to make sure shoppers understand why. Murray says that while one shouldn’t overload on this mineral, clinical evidence suggests calcium supplements that include phosphorus are more effective than those without it.
Meanwhile, boron is said to support bone strength; it facilitates calcium and magnesium absorption and helps reduce urinary calcium excretion, Clow explains.
Heller says in one study, postmenopausal boron-deficient women lost more calcium and magnesium from their bodies than when they were on boron supplementation.
Other minerals, Clow explains, important for bone strength support include:
• Manganese, which enhances bone growth and repair “by stimulating osteoblasts (cells that build bone) and suppressing osteoclasts (cells that break down or resorb bone),” she says.
• Zinc, since deficiency in this mineral may lead to decreased osteoblast levels.
• Copper, which supports bone synthesis.
Moving to vitamins, some of the benefits of vitamin K2 were highlighted earlier. “In my opinion, the role of vitamin K2 is turning out to be one of the most important factors and should be included in every single calcium formulation on the market,” states Topping.
This vitamin helps maintain bone density and move calcium through the bloodstream and into the bones. “It does this by activating two important proteins, osteocalcin and matrix Gla protein (MGP),” says Anderson.
The latter protein is very relevant to heart health, as Anderson explains that MGP stops the accumulation of calcium in the arteries, where calcification can reduce arterial flexibility, vascular health and heart function over time. “Without sufficient K2, MGP cannot perform this duty,” he states.
As for the bones, Heller says postmenopausal women with low vitamin K levels may even be at more risk for increased bone loss than other women. Meanwhile, studies of Japanese women who consumed large amounts of natto—a significant source of K2—found they had fewer incidences of bone fractures. In addition, two one-year studies of vitamin K2 (in the menaquinone-7 [MK-7] form) found that “K2 significantly improved the activation of inert osteocalcin (also called OC carboxylation)” in healthy elderly individuals, according to Anderson. And, findings from a more recent meta-analysis suggest vitamin K2 plays a role in improving vertebral bone mineral density and preventing fractures in postmenopausal women with osteoporosis. “The reduction of undercarboxylated osteocalcin and increment of osteocalcin may have some relation to the process of bone mineralization,” the researchers stated (7).
 There’s more research on MK-7. In a three-year study (8), 244 women took 180 mcg daily of vitamin K2 (as MenaQ7) or a placebo and researchers found “for the first time, clinically statistically significant protection of the vertebrae and the hip (femoral neck) against osteoporosis,” says Anderson. “After three years of supplementation, improvements in both bone mineral content and bone mineral density were statistically significant in the vitamin K2 group. Further, bone strength was statistically improved.”
There’s more research on MK-7. In a three-year study (8), 244 women took 180 mcg daily of vitamin K2 (as MenaQ7) or a placebo and researchers found “for the first time, clinically statistically significant protection of the vertebrae and the hip (femoral neck) against osteoporosis,” says Anderson. “After three years of supplementation, improvements in both bone mineral content and bone mineral density were statistically significant in the vitamin K2 group. Further, bone strength was statistically improved.”
If consumers wonder why K1 is a viable option, Heller believes that K2, especially the MK-7 (menaquinone-7) form, is more bioavailable than K1. Moreover, Anderson says that the 2004 Rotterdam Study (9) found that “high dietary intake of vitamin K2— but not K1—positively impacts cardiovascular health.”
Retailers may also want to alert shoppers taking blood thinners that they should talk to their doctors before taking this supplement.
Other vitamins are important, too. Vitamin C deficiency may be linked with defective bone matrix production, while vitamins B12, B6 and folate promote healthy homocysteine levels, which is important because a high homocysteine level is considered a risk factor for osteoporosis (10).
Levin raises the point that “botanicals hold a lot of promise in aiding bone health.” He points to horsetail (a source of silica); oat straw, alfalfa and nettles for their mineral content; and phytoestrogens from legumes and flax that may support healthy bone matrix.
North American Herb and Spice Co., Lake Forest, IL, says Switzerland’s R.C. Muhlbauer published information in the Journal of Nutrition suggesting that wild, high-mountain spices, like wild rosemary, sage and wild oregano, support bone health (11). “The powers of spice oils and whole spices were dramatic, and it was beyond statistically significant how they blocked bone loss and even resulted in building denser bones,” the firm states.
So in the end, “a bone supplement ‘cocktail,’” as Clouatre calls it, that includes many of the nutrients mentioned in this article may be the best course of action for shoppers looking for bone health support.
Coming Soon
While bone strength is key to a healthy skeletal system, it must always be balanced with flexibility. Stay tuned for next month’s discussion of this topic and supplements that support this key function. WF
References
1. J Nutr Sci Vitaminol (Tokyo). 1999 Oct;45(5):509-17. Calcium absorption from the ingestion of coral-derived calcium by humans.
2. Wolf RL, Cauley JA, Baker CE, et al. Factors associated with calcium absorption efficiency inpre- and perimenopausal women. Am J Clin Nutr 2000; 72: 466-71.
3. National Institutes of Health, “Calcium,” http://ods.od.nih.gov/factsheets/Calcium-HealthProfessional, accessed Apr. 29, 2015.
4. M.J. Bolland, et al., “Calcium Supplements With or Without Vitamin D And Risk Of Cardiovascular Events: Reanalysis Of The Women's Health Initiative Limited Access Dataset And Meta-Analysis,” BMJ. 2011 Apr 19; 342:d2040. doi: 10.1136/bmj.d2040.
5. J.M. Paik, et al., “Calcium Supplement Intake and Risk of Cardiovascular Disease in Women,” Osteoporos Int. 25 (8), 2047–2056 (2014).
6. FAO, “Vitamin D,”www.fao.org/docrep/004/y2809e/y2809e0e.htm, accessed Apr. 29, 2015.
7. Z.B. Huang, et al., “Does Vitamin K2 Play A Role In The Prevention And Treatment Of Osteoporosis For Postmenopausal Women: A Meta-Analysis Of Randomized Controlled Trials,” Osteoporos Int. 26 (3), 1175–1186 (2015).
8. M.H.J. Knapen et al., “Three-Year Low-Dose Menaquinone-7 Supplementation Helps Decrease Bone Loss In Healthy Postmenopausal Women,” Osteoporosis Intl. 24 (9), 2499–2507 (2013).
9. J.M. Geleijnse, et al., “Dietary Intake Of Menaquinone Is Associated With A Reduced Risk Of Coronary Heart Disease: The Rotterdam Study,” J. Nutr. 134 (11), 3100–3105 (2004).
10. Linus Pauling Institute, http://lpi.oregonstate.edu/mic/micronutrients-health/bone-health#table1, accessed Apr. 28, 2015.
11. R.C. Muhlbauer, et al., “Common herbs, essential oils, and monoterpenes potently modulate bone metabolism,” Bone. 32:372 (2003).
12. R.C. Muhlbauer, et al., “Various Selected Vegetables, Fruits, Mushrooms, And Red Wine Residue Inhibit Bone Resorption In Rats,” J. Nutr. 133, 3592–3597 (2010).
Published in WholeFoods Magazine, June 2015











