When life deals us a bad hand, we all go through periods of feeling down, “blah“ or just plain sad. This is completely natural. But when the occasional blues turn into chronic feelings of hopelessness, there could be a problem.
Experts believe that 20% of women and 10% of men may become depressed at some point in their lives (1). Often, those with clinical depression or a diagnosed mood disorder suffer from issues like trouble focusing, fatigue, changes in weight, lack of interest in things/people they once loved and even thoughts of suicide.
Such problems are serious and warrant medical attention. Those who support natural medicine and preventative care believe, however, that much can be done to support a healthy mood before problems start.
Getting to the Gut of Mood Support
Contributing factors to one’s mood range from the psychological to the social. Let’s focus here for a moment on the biological, specifically on neurotransmitters. The brain uses these chemicals to communicate with the nervous system. Nerve cells called neurons are responsible for releasing neurotransmitters that enable the transmission and receipt of messages. Many experts believe that  depression is linked in part to imbalances in neurotransmitters such as serotonin, norepinephrine and dopamine. In fact, several anti-depressant drugs work by affecting these neurotransmitters.
depression is linked in part to imbalances in neurotransmitters such as serotonin, norepinephrine and dopamine. In fact, several anti-depressant drugs work by affecting these neurotransmitters.
The aforementioned neurotransmitters are important to one’s healthy frame of mind. For instance, serotonin is used to make melatonin, a hormone that regulates the sleep cycle. Those having trouble sleeping may have a serotonin deficit; sleep is, of course, important for healing and for a healthy mood. States Neil Levin, CCN, DANLA, nutrition education manager for NOW Foods, Bloomingdale, IL, “Good sleep and healthy melatonin levels are also associated with being able to properly cycle the stress hormone cortisol by reducing its levels at night. That not only helps us to relax and go to sleep, but also allows the adrenal gland to recover and rest overnight, as well.”
Another important role of serotonin is to signal cytokines (i.e., proinflammatory proteins). According to Dallas Clouatre, Ph.D., new product development and marketing consultant for Jarrow Formulas, Los Angeles, CA, when seratonin levels are low—which might be caused by its role in inflammatory processes—one may feel hungry and depressed. “To counteract this, there is a craving for simple sugars and carbohydrates which, when eaten, raise the level of insulin. This increases the relative availability of tryptophan in the blood and serotonin in the brain,” he states. “There is a temporary feeling of well-being from the elevated brain serotonin, but this mood elevation is short-lived as the high insulin now leads to a drop in blood sugar and the cycle is repeated.”
According to David Winston, RH (AHG), founder and president of Herbalist & Alchemist, Washington, NJ, what one eats can affect the way serotonin is made and functions in the body. A lack of protein could inhibit neurotransmitter production, he states, or elevated cortisol levels could negatively affect serotonin production. “A diet that is high in simple carbohydrates certainly can lead to insulin resistance and affect both cortisol and adrenaline and have a negative effect on neurotransmitters as well,” Winston explains.
Other foods to consider are those rich in tryptophan like eggs and milk, since the body makes serotonin during the digestion of this amino acid. “When we eat these foods along with carbohydrates, the tryptophan turns into natural serotonin,” explains Stuart Tomc, CNHP, national educator for Nordic Naturals, Watsonville, CA.
For more on the connection between carbs and mood, see sidebar, “Carbs: The Good, the Bad and the Ugly” on page 28.
 Serotonin and the gut. Serotonin is an interesting neurotransmitter to understand from a nutritional standpoint because it is naturally produced in the gastrointestinal (GI) tract. This serotonin isn’t in a form that can cross the brain–blood barrier, but its precursor compounds made in the gut can reach the brain where additional serotonin is made. Thus, it’s important to note from a nutritional perspective all the ways GI health can affect one’s frame of mind. “When your serotonin levels are normal, you feel good: you sleep and eat well, and you are awake, refreshed, and feel energized. By contrast, a low-serotonin state is one in which you suffer all the symptoms of depression,” says Steve Holtby, president and CEO of Soft Gel Technologies, Inc., Los Angeles, CA. In fact, neurotransmitter depletion and/or surplus is part of what defines depression, says Holtby.
Serotonin and the gut. Serotonin is an interesting neurotransmitter to understand from a nutritional standpoint because it is naturally produced in the gastrointestinal (GI) tract. This serotonin isn’t in a form that can cross the brain–blood barrier, but its precursor compounds made in the gut can reach the brain where additional serotonin is made. Thus, it’s important to note from a nutritional perspective all the ways GI health can affect one’s frame of mind. “When your serotonin levels are normal, you feel good: you sleep and eat well, and you are awake, refreshed, and feel energized. By contrast, a low-serotonin state is one in which you suffer all the symptoms of depression,” says Steve Holtby, president and CEO of Soft Gel Technologies, Inc., Los Angeles, CA. In fact, neurotransmitter depletion and/or surplus is part of what defines depression, says Holtby.
Stomach acids affect neurotransmitters, too. “Because many compounds that affect both anxiety and depression are produced in the GI tract, when herbalists have a patient who is depressed or anxious, they often look at digestive function,” Winston says. “An herbalist will review whether the person is achlorhydric (a lack of stomach acid), hyperchlorhydric (too much stomach acid) or has G.I. dysbiosis with abnormal bowel flora, IBS, a slow transit time or chronic constipation. By helping to normalize bowel health, one can actually, in many cases, normalize neuroendocrine function as well.”
An overall healthy lifestyle can only benefit serotonin production—and this includes getting enough sleep. According to Tomc, one needs at least seven hours of continuous sleep for adequate serotonin production. He names several other contributing lifestyle factors: “All relaxing and meditative activities raise serotonin levels, as does daily exposure to sunlight and daily moderate exercise.”
Supplements and Serotonin
Many of the supplements that line your shelves have a connection to serotonin. According to Jacques d’Anthenaise, chairman of Green Plants Extracts, they fall into two general categories: supplements containing serotonin precursors and those that stimulate the Selection Serotonin Reuptake Inhibitor (SSRI) to help maintain serotonin supplies.
Herbs. For Winston, numerous herbs that support GI health are key for mood support. “Herbalists have long known that we can treat emotional issues through the gut,” he states. Winston names a few herbs that he believes are “top herbs for GI-related depression”: evening primrose (specifically that extracted from the root, leaf and flower), culver’s root and St. John’s wort.
Overall, supporting and strengthening gut function can be a huge help to those affected by low serotonin levels. For this purpose, Winston recommends taking bitter herbs five to 10 minutes before mealtime. “They directly enhance digestion, absorption and elimination, but interestingly enough people who take bitters often will remark that their skin looks better, they have fewer headaches and they have a better overall outlook,” Winston says. “You often get a wide range of affects just by enhancing digestive function.”
Also making the connection between certain herbs, the gut and mood is Grace Ormstein, M.D., CTN, Ph.D., scientific herbal advisor to Himalaya Herbal Healthcare, Houston, TX. She states that her firm makes a supplement with herbs like garcinia, guggul, gymnema and fenugreek that support normal serotonin levels via the digestive tract. Garcinia was chosen because it “promotes normal appetite center function in the brain.”
 That’s not to say all herbs benefit serotonin levels through the GI tract. Others like mucuna, bacopa, gotu kola and jatamansi support normal serotonin levels through the central nervous system, according to Ormstein. “Mucuna, in particular, promotes normal serotonin synthesis,” she states.
That’s not to say all herbs benefit serotonin levels through the GI tract. Others like mucuna, bacopa, gotu kola and jatamansi support normal serotonin levels through the central nervous system, according to Ormstein. “Mucuna, in particular, promotes normal serotonin synthesis,” she states.
And, Winston explains that depression is sometimes related to the liver, a condition he calls hepatic depression. “The person has a bilious, sour attitude, a sour stomach, flies off the handle in anger,” Winston says, noting that rosemary and white peony may help.
Omegas. A poor balance of omega-3s to omega-6s can work against individuals’ adequate production and use of serotonin. Tomc raises the point that for serotonin to function properly, it must pass through cell membranes—and this can’t be done with rigid, unhealthy cell walls. He explains that omega-3s help make cell membranes permeable; conversely, a lack of this essential fatty acid makes cell walls far less fluid.
“This is a considerable problem, given that even the healthiest diets rarely provide adequate amounts of omega-3s,” Tomc states. “Research is still needed on the exact mechanisms involved, but we do know that increasing omega-3 has direct effects on serotonin levels.” Psychiatrist Joseph Hibbeln, M.D., from the National Institute of Health, Tomc says, believes a lack of omega-3s in most Americans’ diet is a contributing factor for the rise of depression in the United States.
In fact, Elizabeth Somer, M.A., R.D., author of Eat Your Way to Happiness, says studies indicate those who are depressed and women with postpartum depression “have much lower DHA levels in their blood, fat tissues and cerebrospinal fluids—up to 36% lower than happy  people.” She sums it up like this: when DHA levels drop, so too do serotonin levels, “leaving people grumpy, blue, and even depressed… The more DHA your brain has, the more flexible your brain cells become. The more flexible your brain cells become, the better you think and the better you feel!”
people.” She sums it up like this: when DHA levels drop, so too do serotonin levels, “leaving people grumpy, blue, and even depressed… The more DHA your brain has, the more flexible your brain cells become. The more flexible your brain cells become, the better you think and the better you feel!”
The link to DHA isn’t just about depression. Some believe that this omega-3 fatty acid can help those with chronic aggressive or hostile behavior. And, there’s been some research on children, too. “Researchers at Purdue University found that children with low omega-3 levels are most likely to throw tantrums, have sleep problems and battle learning disabilities, while kids who are optimally nourished in these fats are least prone to attention deficit disorders. Even convicts in prison are less aggressive and angry when they take omega-3 supplements,” Somer says.
 This underscores the importance of getting enough DHA from the diet and through supplementation with fish oil or vegetarian DHA. Says Tomc, “DHA is absolutely critical for a well-functioning brain, affecting how fast and efficient the brain cells pass information and assisting in the making and repairing of brain cells. Better brain function and reduced mood disorders are all positively associated with omega-3 fats.”
This underscores the importance of getting enough DHA from the diet and through supplementation with fish oil or vegetarian DHA. Says Tomc, “DHA is absolutely critical for a well-functioning brain, affecting how fast and efficient the brain cells pass information and assisting in the making and repairing of brain cells. Better brain function and reduced mood disorders are all positively associated with omega-3 fats.”
Amino acids. Previously, we mentioned that eating tryptophan-rich foods may aid in maintaining proper serotonin levels. But, Levin makes the point that we may not want to rely on food alone for this purpose. He says the body can only use a small amount of this amino acid for making serotonin since it must use it for other purposes like making muscle.
Thus, he notes that l-tryptophan and its metabolite 5-HTP are both available as dietary supplements, and requires less intake than dietary tryptophan. “A 500-mg serving of tryptophan is about equivalent to 50-mg of 5-HTP in terms of how much 5-HTP the body will normally produce from that much tryptophan,” he states.
Vitamins and minerals. Jack Challem, author of The Food-Mood Solution (Wiley, 2007) and a formulator of Mellow Mood for Carlson Labs, Arlington Heights, IL, says while serotonin (like most neurotransmitters) is built from amino acids, they also “depend on vitamins and minerals for the enzymatic reactions that convert the amino acids to full-fledged neurotransmitters.”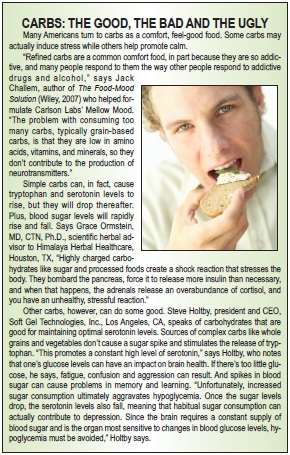
Serotonin, for instance, not only requires L-tryptophan, but also vitamin B6 (which converts L-tryptophan or 5-HTP to serotonin), Challem states. “Low levels of these nutrients can interfere with serotonin production, and sometimes genetic issues limit how well people make serotonin,” he adds.
Also speaking of the B-vitamins is Daemon Jones, N.D., a naturopathic physician and member of the Nutritional Magnesium Association. He says that folic acid, for instance, helps stabilize mood by working with serotonin. Though its role on this front is not completely understood, Jones notes that it may act though S-Adenosyl methionine (SAMe), a compound found in nearly every tissue in the body.
The B-vitamins are also known to help with energy at the cellular level, which is important, says Challem, because those with depression often lack energy. He adds that “large amounts of some B-vitamins, such as niacin or niacinamide, combined with large amounts of vitamin C, are very helpful in recent-onset schizophrenia.”
d’Anthenaise offers this cheat sheet for how B-vitamins affect mood:
• B2: effective on the central nervous system and memory.
• B3: wellbeing of nervous system, neurotransmitters and memory troubles
• B5: nervous system support and anti-stress effect
• B6: nervous disorders
• B8: nerves protection
• B9: wellbeing of nervous system
And, Emek Blair, Ph.D., director of R&D at Empirical Labs, Fort Collins, CO, says that B12 is especially helpful for children’s cognitive development. “It is likely that it continues to play an important role throughout our lives. Oftentimes, doctors will also prescribe a B complex along with anti-depression medication. Also, B6 is thought to be integral in serotonin production.”
But Levin cautions us to be not think of these vitamins in a singular fashion. He states, “It is wise to get the full spectrum of B vitamins, as many of them function in groups rather than singly. For example, three B vitamins are required to metabolize the undesirable metabolite homocysteine back to the amino acid methionine. Homocysteine elevation also indicates that this chemical is not properly generating the important antioxidants cysteine and glutathione from methionine, thus increasing the risk of cellular and tissue damage in the body.”
There’s more to the picture than the Bs. According to Holtby, specific vitamins known to support healthy serotonin levels include selenium and vitamin D, which “increase the enzyme supply that converts certain amino acids into serotonin.”
Retailers must also be sure to point out to shoppers that magnesium is important in the serotonin story, says Carolyn Dean, M.D., N.D., medical director of the Nutritional Magnesium Association. She states that magnesium is necessary for serotonin production and function, which is important to note since stress depletes the body’s stores of this essential mineral. “A person that is going through a stressful period without sufficient magnesium can set up a deficit that, if not corrected, can linger, causing depression and further health problems,” Dean believes, adding, “The body needs magnesium in order to release and bind adequate amounts of serotonin in the brain for balanced mental functioning.”
Stressed Out?
Dealing with chronic stress is a major—and unfortunately too common—contributing factor in mood disorders. Says Kevin Tofts, president of Gemini Nutraceuticals LLC, Westwood, NJ, “In today’s environment, a person’s mood and his/her ability to deal with stress has become extremely important. The world today is stressful and people need a natural way to help them deal with the stress of everyday life.”
The cortisol connection. The hormone cortisol is another factor is one’s mood thanks to its role in stress. Chronic stress could be a risk factor in developing depression or emotional problems if one doesn’t cope with stress well (2).
In response to stressors, the body secretes adrenaline to help with the fight-or-flight reaction, and the hormone cortisol is secreted to help the brain use glucose and to repair tissue. To help reserve functions not critical for fight-or-flight, cortisol alters immune, digestive and reproductive system processes. “This complex natural alarm system also communicates with regions of your brain that control mood, motivation and fear,” says the Mayo Clinic (3).
If these responses are constantly in motion thanks to chronic stress, the mind and body could suffer. For instance, depression is often associated with high levels of cortisol and stress increases one’s need for serotonin. In general, supporting adrenal health may be key in coping with stress and associated mood disorders.
“Being able to counter excess or chronic cortisol production in response to stress is important since excess cortisol can not only interfere with our ability to relax, but also may encourage stress-related overeating and the accumulation of abdominal fat,” states Levin.
One of the many nutrients that addresses this issue is a branded plant extract that combines Magnolia officinalis and Phellodendron amurense (Relora), Levin states. The trademarked ingredient, he says, “can help to alleviate symptoms associated with stress such as nervous tension, irritability, concentration difficulties and occasional sleeplessness” while also helping to “control appetite and prevent stress-related eating, aiding in weight control.”
Other supplements that may help balance melatonin levels and reduce the affect of increased cortisol levels, says Holtby, include the B-vitamins (B6, B12 and folate), chromium picolinate, essential fatty acids, phosphorylated serine and DHEA.
On the anti-stress front, Levin reminds us that l-theanine promotes relaxation while taurine “helps to digest fats, regulate heart beat, maintain cell membrane stability, and prevent excessive brain cell activity.”
But, Blair states that maintaining proper cortisol levels is also a matter of diet and the timing of one’s meals. “After fasting for eight hours due to sleep, your body responds by increasing cortisol levels to help generate energy (its intended function). A great way to reduce stress is to eat breakfast immediately after waking up to lower cortisol levels,” he states.
Calmness and calcium. Having an appropriate ratio of calcium to magnesium is important for a healthy calm state (and other health functions). Shoppers are well-versed in calcium’s bone health properties, but the calcium–magnesium ratio (2:1) is far less well known. Ken Whitman, president of Natural Vitality, Austin, TX, says that many women follow their doctors’ orders to take 1,000–1,200 mg of calcium every day. But, he believes “many women don’t consider calcium already in their diet and look to supplemental calcium to make up these numbers. This will result in a very high calcium diet which in itself is one of the causes of magnesium depletion.”
Says Kristy L. Anderson, NMD, medical advisor of bioregulatory medicine to Heel USA, Albuquerque, NM, “Most consumers read about isolated botanical, homeopathic or nutritional supplements and they think that if they take those isolated constituents that they will achieve optimal health. However, this is not always the case and sometimes this can be detrimental because taking isolated constituents may imbalance other levels in the body and lead to unwanted effects in health.”
So, what’s the connection between calcium–magnesium and stress? According to Holtby, magnesium helps muscles to relax while calcium makes them contract. He states, “Too little balance between magnesium and calcium can be both uncomfortable and unhealthy. The combination of these two minerals has effects as a natural tranquillizer. The demand for magnesium goes up with stress.”
But, too much calcium can make magnesium absorption tough. Winston says magnesium deficiency is so common that he often tells patients they should have a 1:1 ratio of calcium to magnesium. He states, “Most Americans are probably getting enough calcium; what they’re not getting is enough magnesium.”
Some experts interviewed for this piece, like Dean, says we should focus on getting calcium from food. Supplementation should be considered after one determines how much calcium is consumed through dietary means. Then, calcium supplements should be a few hundred milligrams for most healthy individuals, says Clouatre. Plus, “Calcium supplements should be slow-release forms and be accompanied by supporting minerals, such as magnesium, manganese, zinc, vitamin D, etc. Bone-derived microcrystalline hydroxyapatite is an excellent calcium source because of its balance and its proper controlled release of calcium into the system.”
Relaxing herbs. Many shoppers love to use herbs to restore a healthy mood. WholeFoods asked those interviewed for this piece to identify their top three most important calming herbs for retailers to stock. Here’s what they had to say, though Winston reminds us that there are numerous calming herbs, and just the handful presented here won’t necessarily work for everyone.
• Valerian root topped the list of favorites. This herb is said to be useful as a sleep aid and for tension/anxiety support.
• Another popular choice was passionflower. Winston believes this herb is good for those with “busy minds” who have trouble sleeping and achieving calmness in general. “It is especially useful for people who, when they are under stress, develop symptoms such as stress-induced arrhythmias, stress-induced IBS or palpitations,” he adds.
• Eileen Sheets, managing director for Bioforce USA, Ghent, NY speaks of Avena sativa, a fresh, flowering oat. Sheets explains that this herb is “one of the best remedies to nourish the exhausted nervous system, particularly during stressful periods. One of its more modern uses is as part of a treatment plan for addiction. It is being used to help the nervous system through withdrawal.”
Winston seconds the idea of oat extract, specifically that made from fresh milky oat seed. “In my mind, this is one of our greatest nerve trophorestoratives. Think of it as a food for the nervous system,” says Winston, adding, “Fresh oat is for people who burn the candle at both ends, the top, the bottom, the sides and the middle. They are so fried, they are crispy. These people become emotionally labile; they have lost their emotional foundation.” While he admits that it takes some time to be effective, this extract will help rebuild the emotional foundation over time. This makes sense since he says, “Stress takes its toll over a long period and likewise, this should be taken over a period of months to rebuild and restore one’s emotional foundation.”
In fact, Anderson of Heel USA notes that the three aforementioned herbs are combined in her company’s proprietary homeopathic blend that is said to help the body adapt to stress (Neurexan). Speaking of our first three herbs, she states, “They are also generally safe to use for most people with a variety of conditions with few limitations or possible contraindications.”
• Skullcap is beneficial for anxiety support. The American variety, according to Winston, is especially helpful for those who are stressed out and fidgety. This herb also works over time, as opposed to offering fast relief.
• St. John’s wort is said to support a healthy mood, but Levin warns that it shouldn’t be used with prescription mood drugs and can interact with other drugs. One year-long study sponsored by Bioforce found that St. John’s wort (from A. Vogel) reduced the severity of depression by 54%, anxiety by 49% and nervousness by 50%, according to Eileen Sheets, managing director for Bioforce USA, Ghent, NY. “Along with addressing anxiety and depression, this study showed A. Vogel St. John’s wort nicely addresses the physical symptoms that can be a part of depression,” she says.
• Chamomile is well-known for its calming properties.
• Also key in this category is kava, which helps with mental focus and muscle relaxation, according to Levin.
• A branded extract of the Chinese herb Apocynum venetum (Posinol from Soft Gel Technologies) “promotes a positive mental outlook by supporting a healthy balance of neurotransmitters,” says Holtby. In studies, the herb was found to increase serotonin levels.
• Ormstein recommends two more herbs: bacopa (which she says “promotes mental alertness in people who experience an occasional lack of attention span and want to improve their frustration tolerance”) and gotu kola.
• Last is saffron, which d’Anthenaise says has been studied for its effects on stress and emotional balance. Of note, he says that this herb helps stimulate selection serotonin reuptake inhibitor. In studies, a branded saffron extract (Saffr’ Activ from Gemini Nutraceuticals) was found to help increase serotonin levels, according to Tofts. He adds that a placebo-controlled study found the extract “decreased the intensity of stress measured in saffron-treated patients (30 mg/day) as compared to those who received a placebo.” Of note, he says the herb has similar positive effects as two prescription antidepressant drugs (imipramsine and fluoxetine like Prozac)—without side effects.
Many of these herbs are found in combination products, and for good reason, according to Blair. He believes combinations of herbs can actually increase their efficacy. Plus, “By taking less of each ingredient, we are less likely to become sensitized, as opposed to taking large amounts of a single ingredient,” Blair feels. WF
References
1. R. Nemade, N. Staats Reiss and M. Dombeck, “Depression: Major Depression & Unipolar Varieties,” updated 2007, www.mhcinc.org/poc/view_doc.php?type=doc&id=12978&cn=5, accessed April 2, 2011.
2. “How Stress, Anxiety, and Depression Affect Your Health,” www.webmd.com/depression/stress-anxiety-depression, accessed April 9, 2011.
3. “Stress: Constant Stress Puts Your Health at Risk,” http://www.mayoclinic.com/health/stress/SR00001, accessed April 9, 2011.
Published in WholeFoods Magazine, July 2011